This new interview in the Changemakers series explores the journey from solo home visits to building a national palliative care system; strategic thinking and honest effort within constraints; forming alliances with officials, international organisations, doctors, and rural communities; the significance of mentors and inspiring role models, and a strong belief in the value of every human life.
PACED team member Ira Chernozhukova spoke with Taalaigul Sabyrbekova, a phthisiatrician, public advocate, and Co-Chair of the Palliative and Hospice Care Association of Kyrgyzstan. Taalaigul has played a key role in the development of palliative care in the country, contributing to systemic change, training of specialists, the creation of legal frameworks, and the emergence of a new professional community.
Читайте на русском языке.
PACED team member Ira Chernozhukova spoke with Taalaigul Sabyrbekova, a phthisiatrician, public advocate, and Co-Chair of the Palliative and Hospice Care Association of Kyrgyzstan. Taalaigul has played a key role in the development of palliative care in the country, contributing to systemic change, training of specialists, the creation of legal frameworks, and the emergence of a new professional community.
Читайте на русском языке.
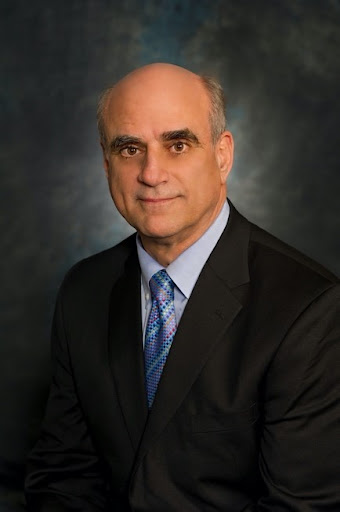
Stephen R. Connor
PhD – clinical health psychologist, palliative care consultant, and executive director of the Worldwide Hospice and Palliative Care Alliance (WHPCA)

Maral Turdumatova
Paediatric palliative care physician and lead specialist of the multidisciplinary team at the Public Charitable Foundation “First Children's Hospice” in Bishkek, Kyrgyzstan.

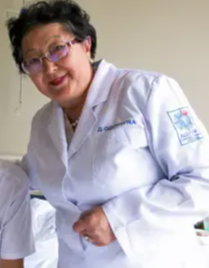
Olga Viktorovna Mychko
an oncologist and Chief External Specialist for Palliative Medical Care (adult population) at the Ministry of Health of the Republic of Belarus.
Odontuya Davaasuren
MD, PhD, Professor at the Department of General Practice and Basic Clinical Skills, Mongolian National University of Medical Sciences, Ulaanbaatar, Mongolia.

Anna Konstantinovna (Nyuta) Federmesser
Russian public figure and founder of the Vera Hospice Charity Fund.
Sechenov First Moscow State Medical University.

Milana Turgunalieva
Co-Chair of the Palliative and Hospice Care Association of Kyrgyzstan.
Ira: Why did you decide to pursue medicine? And how did you find yourself in such a relatively new and intricate field as palliative care?
Taalaigul: I decided I wanted to become a doctor while still at school. I enrolled in medical school, qualified as a phthisiatrician, and began working in the Department of Phthisiology. My patients were individuals suffering from tuberculosis. After the fall of the Soviet Union, we started to encounter forms of TB that, according to senior colleagues, hadn't been seen since World War II—severe, neglected cases with virtually no medication available. The situation was dire.
Some time later, life led me to a humanitarian organisation involved in medicine supply. That’s where I started developing professionally in healthcare systems management. It was then that I realised: access to medicines is not just about logistics, it reflects the state of the entire health system.
Taalaigul: I decided I wanted to become a doctor while still at school. I enrolled in medical school, qualified as a phthisiatrician, and began working in the Department of Phthisiology. My patients were individuals suffering from tuberculosis. After the fall of the Soviet Union, we started to encounter forms of TB that, according to senior colleagues, hadn't been seen since World War II—severe, neglected cases with virtually no medication available. The situation was dire.
Some time later, life led me to a humanitarian organisation involved in medicine supply. That’s where I started developing professionally in healthcare systems management. It was then that I realised: access to medicines is not just about logistics, it reflects the state of the entire health system.
If a country is reforming its healthcare system, access to medicine must be included in the agenda.
Later, my colleagues and I founded the Public Charity Ergene to address issues related to access to food and medicines. I attended a conference supporting women with breast cancer, and it was then that I first realised the extent of the problem. At that time, I knew very little about oncology.
We discovered that in Kyrgyzstan, breast cancer was the most common cancer in both incidence and mortality (as of 2007). There was no proper diagnosis, no laboratories to determine the hormonal status of tumours. Women were treated blindly, purchasing drugs themselves without knowing whether they were suitable or not. We began drafting project proposals and seeking funding. At that time, donors were not interested in cancer — their focus was on TB, HIV, maternal and child health.
The Swiss Embassy in Kyrgyzstan supported our project by providing funding to establish the country’s first immunohistochemistry lab for early diagnosis. This was a significant milestone. However, women started coming to us with stage 3–4 breast cancer, and we found ourselves unable to help them. That was when one of my colleagues first mentioned palliative care to me.
We analysed the situation and prepared a report showing that palliative care in Kyrgyzstan essentially did not exist. That was in 2009. For me as a doctor, it was an entirely new topic, but I gradually started to understand what it meant. I learned that Open Society was supporting palliative care in other countries, and I reached out to the Soros Foundation Kyrgyzstan — but the project wasn’t active in our country yet. They only began funding the first palliative care programme in 2011.
Building something as complex as palliative care without funding, relying solely on enthusiasm, is incredibly challenging. Therefore, the project launched in 2011 gave us real momentum. That same year, the first needs assessment was conducted. Its author was Dr. Stephen Connor, who now leads the Worldwide Hospice and Palliative Care Alliance.
We still utilise the needs assessment framework from that report — it became a powerful tool in our dialogue with the state: ‘Look how many people in this country need palliative care!’ I was chosen for a programme at the University of Wisconsin — the Pain & Policy Studies Group, which concentrated on global pain management policy. I studied remotely for two years. The most important thing I learnt was how to assess access to morphine and other opioids.
We formed a working group comprising representatives from the Ministry of Health, the Mandatory Health Insurance Fund, the Department of Pharmaceutical Supply, the Drug Control Agency, oncologists, and many others. We came together to assess our current position and resources.
We also carried out our own sociological research. In one survey, we visited family medicine centres and asked: ‘If a person has late-stage cancer, is it normal for them to be in pain?’
We discovered that in Kyrgyzstan, breast cancer was the most common cancer in both incidence and mortality (as of 2007). There was no proper diagnosis, no laboratories to determine the hormonal status of tumours. Women were treated blindly, purchasing drugs themselves without knowing whether they were suitable or not. We began drafting project proposals and seeking funding. At that time, donors were not interested in cancer — their focus was on TB, HIV, maternal and child health.
The Swiss Embassy in Kyrgyzstan supported our project by providing funding to establish the country’s first immunohistochemistry lab for early diagnosis. This was a significant milestone. However, women started coming to us with stage 3–4 breast cancer, and we found ourselves unable to help them. That was when one of my colleagues first mentioned palliative care to me.
We analysed the situation and prepared a report showing that palliative care in Kyrgyzstan essentially did not exist. That was in 2009. For me as a doctor, it was an entirely new topic, but I gradually started to understand what it meant. I learned that Open Society was supporting palliative care in other countries, and I reached out to the Soros Foundation Kyrgyzstan — but the project wasn’t active in our country yet. They only began funding the first palliative care programme in 2011.
Building something as complex as palliative care without funding, relying solely on enthusiasm, is incredibly challenging. Therefore, the project launched in 2011 gave us real momentum. That same year, the first needs assessment was conducted. Its author was Dr. Stephen Connor, who now leads the Worldwide Hospice and Palliative Care Alliance.
We still utilise the needs assessment framework from that report — it became a powerful tool in our dialogue with the state: ‘Look how many people in this country need palliative care!’ I was chosen for a programme at the University of Wisconsin — the Pain & Policy Studies Group, which concentrated on global pain management policy. I studied remotely for two years. The most important thing I learnt was how to assess access to morphine and other opioids.
We formed a working group comprising representatives from the Ministry of Health, the Mandatory Health Insurance Fund, the Department of Pharmaceutical Supply, the Drug Control Agency, oncologists, and many others. We came together to assess our current position and resources.
We also carried out our own sociological research. In one survey, we visited family medicine centres and asked: ‘If a person has late-stage cancer, is it normal for them to be in pain?’
25% of respondents replied: ‘Yes, that’s normal. Pain is part of the illness. You just have to endure it, it’s nothing terrible.’
That was when we realised: we needed to change the way people think. We needed to talk about life without pain, because that is an essential part of palliative care. No one should suffer, not even in the terminal stage. We began speaking on television and radio, organised charity concerts, and tried to raise funds for morphine. But all of that had little effect.
The most important thing is for doctors to genuinely understand what palliative care is, and for there to be no regulatory obstacles.
Our working group began reviewing all the decrees and regulations related to pain medications, prescriptions, and drug dispensing. We discovered that the key to solving many issues was hidden there. So we started working in that direction.
Ira: Why did you specifically focus on palliative care, and not, for instance, on oncology?
Taalaigul: Initially, palliative care seemed very different from what I was used to. Doctors are trained to cure. Many of my colleagues still believe we must fight for a patient until the very end, and that palliative care means giving up. But I saw genuine compassion in it—helping someone when they are at their most vulnerable. That, to me, is the essence of palliative care.
I also had a personal experience. My father, an elderly man, needed care during the last three years of his life. Everything I had learned, I applied then. I knew how to feed him, how not to force him to eat, how to assess pain levels, and how to relieve symptoms. I believe we provided him with proper and dignified care.
Previously, it was like this: someone receives a devastating diagnosis, and the doctor says, ‘There’s nothing we can do.’ And that’s it—silence, emptiness. At one meeting, a colleague from Armenia said, ‘I’m proud that I can help someone until their last breath.’
I gained knowledge gradually through conversations with colleagues from other countries, with patients, and with families. At one Soros Foundation conference in Kyrgyzstan, there were experts from Georgia. One of them said, ‘You must never force someone to eat if they don’t want to.’ Next to me sat a lecturer from the Kyrgyz Institute for Advanced Medical Training, and I heard her whisper to herself: ‘God… the mistakes I made when I was caring for my father. Why did I force him to eat?’
Many of those mistakes could have been prevented.
Ira: What do you say when someone asks what your profession is?
Taalaigul: I say that I work with the Palliative and Hospice Care Association, and sometimes I notice surprise or confusion in their eyes. Then I explain: ‘It’s care focused on supporting people with the most serious illnesses, with incurable diagnoses.’ Usually, that’s enough. People nod, they understand.
Sometimes, when I speak to people in villages and they ask what kind of doctor I am, I usually say I’m a lung specialist—that’s my original speciality—and that I also work on developing care for the most seriously ill patients. That’s usually enough as well.
Ira: It appears that even among doctors, not everyone is familiar with the term ‘palliative care.’
Taalaigul: Yes, absolutely. Many people hear about it for the first time from us. Even those who are familiar with it often do not fully understand what it truly means. Some believe it’s only related to the terminal stage of cancer. Others think palliative care is what occurs ‘when medicine can no longer help.’ There are many myths and misconceptions.
Ira: If you could dispel one myth about palliative care, what would it be?
Taalaigul: I would say this: sending someone home with the words, ‘There’s nothing more we can do,’ is unacceptable. We may not be able to cure, but we can ensure that the person does not suffer. That is palliative care.
Thanks to palliative care, I’ve changed my view on death. Or perhaps that realisation only came with time.
Ira: Why did you specifically focus on palliative care, and not, for instance, on oncology?
Taalaigul: Initially, palliative care seemed very different from what I was used to. Doctors are trained to cure. Many of my colleagues still believe we must fight for a patient until the very end, and that palliative care means giving up. But I saw genuine compassion in it—helping someone when they are at their most vulnerable. That, to me, is the essence of palliative care.
I also had a personal experience. My father, an elderly man, needed care during the last three years of his life. Everything I had learned, I applied then. I knew how to feed him, how not to force him to eat, how to assess pain levels, and how to relieve symptoms. I believe we provided him with proper and dignified care.
Previously, it was like this: someone receives a devastating diagnosis, and the doctor says, ‘There’s nothing we can do.’ And that’s it—silence, emptiness. At one meeting, a colleague from Armenia said, ‘I’m proud that I can help someone until their last breath.’
I gained knowledge gradually through conversations with colleagues from other countries, with patients, and with families. At one Soros Foundation conference in Kyrgyzstan, there were experts from Georgia. One of them said, ‘You must never force someone to eat if they don’t want to.’ Next to me sat a lecturer from the Kyrgyz Institute for Advanced Medical Training, and I heard her whisper to herself: ‘God… the mistakes I made when I was caring for my father. Why did I force him to eat?’
Many of those mistakes could have been prevented.
Ira: What do you say when someone asks what your profession is?
Taalaigul: I say that I work with the Palliative and Hospice Care Association, and sometimes I notice surprise or confusion in their eyes. Then I explain: ‘It’s care focused on supporting people with the most serious illnesses, with incurable diagnoses.’ Usually, that’s enough. People nod, they understand.
Sometimes, when I speak to people in villages and they ask what kind of doctor I am, I usually say I’m a lung specialist—that’s my original speciality—and that I also work on developing care for the most seriously ill patients. That’s usually enough as well.
Ira: It appears that even among doctors, not everyone is familiar with the term ‘palliative care.’
Taalaigul: Yes, absolutely. Many people hear about it for the first time from us. Even those who are familiar with it often do not fully understand what it truly means. Some believe it’s only related to the terminal stage of cancer. Others think palliative care is what occurs ‘when medicine can no longer help.’ There are many myths and misconceptions.
Ira: If you could dispel one myth about palliative care, what would it be?
Taalaigul: I would say this: sending someone home with the words, ‘There’s nothing more we can do,’ is unacceptable. We may not be able to cure, but we can ensure that the person does not suffer. That is palliative care.
Thanks to palliative care, I’ve changed my view on death. Or perhaps that realisation only came with time.
I realised that we are not afraid of death—we are afraid of the suffering that comes with it. And palliative care is not about death; it is about life.
Taalaigul with colleagues / Personal photo archive
We had a case where a patient couldn’t forgive his mother, and a doctor helped him overcome that resentment. In other cases, family members blamed a wife for her husband’s illness. Then a doctor came, praised her for how she was caring for him, and the blame disappeared.
Everyone affected by palliative care experiences relief, both physically and emotionally. Palliative care is not just a single service; it is a comprehensive system. And you cannot isolate any part of it. Everything is interlinked.
Ira: What other challenges have you encountered?
Taalaigul: At one point, Dr. Maral and I realised we simply didn’t have enough hands, especially for basic caregiving. At the time, we were making home visits supported by the Soros Foundation and prioritising patients who had absolutely no help, no relatives, no carers.
We asked ourselves: where can we find people who can simply help feed someone, help them wash, and bring what they need? We reached out to a local church, made an agreement, and volunteers began visiting our patients — sometimes just to help wash their hair. Simple acts, but very important. Then we approached the Muftiate and asked imams to speak during Friday prayers, to explain that no one should have to suffer. That was our way of trying to raise awareness.
When I was a medical student, we weren’t taught anything about palliative care. No one discussed morphine or suffering in the final stages of life. At most, we learned about rehabilitation, and even then, it was like: ‘Take them home, and goodbye.’
Technically, morphine was available and could be prescribed. However, we later found out that after Kyrgyzstan gained independence, the country faced a serious drug trafficking problem, leading to the implementation of strict drug control laws. These laws affected not only illegal substances but also legitimate medications. As a result, access to pain relief became nearly impossible: a maximum of 10 ampoules per prescription, prescriptions valid only until a certain hour, mandatory certificates, and official registration of the patient.
Everyone affected by palliative care experiences relief, both physically and emotionally. Palliative care is not just a single service; it is a comprehensive system. And you cannot isolate any part of it. Everything is interlinked.
Ira: What other challenges have you encountered?
Taalaigul: At one point, Dr. Maral and I realised we simply didn’t have enough hands, especially for basic caregiving. At the time, we were making home visits supported by the Soros Foundation and prioritising patients who had absolutely no help, no relatives, no carers.
We asked ourselves: where can we find people who can simply help feed someone, help them wash, and bring what they need? We reached out to a local church, made an agreement, and volunteers began visiting our patients — sometimes just to help wash their hair. Simple acts, but very important. Then we approached the Muftiate and asked imams to speak during Friday prayers, to explain that no one should have to suffer. That was our way of trying to raise awareness.
When I was a medical student, we weren’t taught anything about palliative care. No one discussed morphine or suffering in the final stages of life. At most, we learned about rehabilitation, and even then, it was like: ‘Take them home, and goodbye.’
Technically, morphine was available and could be prescribed. However, we later found out that after Kyrgyzstan gained independence, the country faced a serious drug trafficking problem, leading to the implementation of strict drug control laws. These laws affected not only illegal substances but also legitimate medications. As a result, access to pain relief became nearly impossible: a maximum of 10 ampoules per prescription, prescriptions valid only until a certain hour, mandatory certificates, and official registration of the patient.
We began scrutinising each restriction point and seeking ways to ease them. It took years, but now some of these barriers have been removed. It is vital that doctors are informed about these changes and feel confident to prescribe morphine.
My role here is to advocate for systemic reform.
According to the International Narcotic Control Board's formula, Kyrgyzstan requires about 16–18 kilograms of morphine annually—the minimum necessary based on population and palliative care needs. We still use less than one kilogram, and it was even lower before, just 200 grams per year. This shows that for many, pain remains unrelieved.
Most doctors still rely on non-steroidal anti-inflammatory drugs to manage pain, or, at best, tramadol. However, last year, tramadol was classified as a controlled substance and now requires a special kind of prescription. As a result, the situation remains challenging.
For a long time, we didn’t even have a clinical protocol for delivering palliative care. In 2013, we once again assembled a working group and started developing a guideline. We lacked qualified specialists in this field—there was simply no such thing as a certified palliative care doctor in the country. So, we took responsibility ourselves. Fortunately, our colleagues committed to evidence-based medicine supported us.
According to the International Narcotic Control Board's formula, Kyrgyzstan requires about 16–18 kilograms of morphine annually—the minimum necessary based on population and palliative care needs. We still use less than one kilogram, and it was even lower before, just 200 grams per year. This shows that for many, pain remains unrelieved.
Most doctors still rely on non-steroidal anti-inflammatory drugs to manage pain, or, at best, tramadol. However, last year, tramadol was classified as a controlled substance and now requires a special kind of prescription. As a result, the situation remains challenging.
For a long time, we didn’t even have a clinical protocol for delivering palliative care. In 2013, we once again assembled a working group and started developing a guideline. We lacked qualified specialists in this field—there was simply no such thing as a certified palliative care doctor in the country. So, we took responsibility ourselves. Fortunately, our colleagues committed to evidence-based medicine supported us.
That year, the Ministry of Health approved the first palliative care guideline and a clinical protocol for managing chronic pain.
I learned a great deal throughout the process. Dr. Stephen Connor recommended a fantastic resource—the Pallcare Book. It’s continually updated, and I still use it today—reading, checking, and cross-referencing. It has become a true companion in my work.
We printed the protocol in large quantities—again with support from the Soros Foundation—and distributed it to primary care doctors. That was a milestone: for the first time, frontline physicians had a guideline officially approved by the Ministry of Health, a document they could rely on. It was a genuine breakthrough.
Every ten years, we review and update our protocol to expand its scope. For instance, for a patient to be granted ‘palliative status,’ primary care doctors must refer them to Bishkek or another major centre where a specialist (such as a pulmonologist or cardiologist) makes the final diagnosis: organ failure, cancer stage, and so on. Only then can a patient be officially registered as palliative.
Now, our aim is to enable local doctors in the regions to identify palliative patients themselves, establish the diagnosis, record it, and start symptom management. And—this is so important—to be able to communicate this information to the patient and their family openly, gently, and with understanding.
We’ve developed standard operating procedures (SOPs), and now it’s time to implement them. That’s why we require cooperation with postgraduate training institutions, in-depth courses, and specialised approaches. The moment to progress has arrived.
Ira: Is palliative care covered by Kyrgyzstan’s legal framework?
Taalaigul: In 2016, Kyrgyzstan included a section on palliative care in the Law ‘On Public Health’. In 2024, the country underwent a major legislative reform: a new consolidated law was enacted, bringing together all existing health regulations, and it includes a specific clause dedicated to palliative care. It clearly states that palliative care must be available at all levels—from pre-medical to specialised care.
This provided us with a solid foundation to progress and start developing the formal procedures for delivering palliative care, as these are still not fully outlined. We need clear definitions: who determines a patient’s palliative status, and what criteria, tests, and diagnostics are required.
We were all born once, and we will all eventually leave this world. Just as we care deeply about the conditions under which a child is born—we have maternity hospitals, prenatal care, and an entire system—we must also care about the circumstances in which a person dies.
Ira: What advice would you give to colleagues in other countries with limited resources who are also striving to develop palliative care amid shortages of staff, knowledge, and medicines?
Taalaigul: Of course, you always have to ‘look in your wallet.’
We printed the protocol in large quantities—again with support from the Soros Foundation—and distributed it to primary care doctors. That was a milestone: for the first time, frontline physicians had a guideline officially approved by the Ministry of Health, a document they could rely on. It was a genuine breakthrough.
Every ten years, we review and update our protocol to expand its scope. For instance, for a patient to be granted ‘palliative status,’ primary care doctors must refer them to Bishkek or another major centre where a specialist (such as a pulmonologist or cardiologist) makes the final diagnosis: organ failure, cancer stage, and so on. Only then can a patient be officially registered as palliative.
Now, our aim is to enable local doctors in the regions to identify palliative patients themselves, establish the diagnosis, record it, and start symptom management. And—this is so important—to be able to communicate this information to the patient and their family openly, gently, and with understanding.
We’ve developed standard operating procedures (SOPs), and now it’s time to implement them. That’s why we require cooperation with postgraduate training institutions, in-depth courses, and specialised approaches. The moment to progress has arrived.
Ira: Is palliative care covered by Kyrgyzstan’s legal framework?
Taalaigul: In 2016, Kyrgyzstan included a section on palliative care in the Law ‘On Public Health’. In 2024, the country underwent a major legislative reform: a new consolidated law was enacted, bringing together all existing health regulations, and it includes a specific clause dedicated to palliative care. It clearly states that palliative care must be available at all levels—from pre-medical to specialised care.
This provided us with a solid foundation to progress and start developing the formal procedures for delivering palliative care, as these are still not fully outlined. We need clear definitions: who determines a patient’s palliative status, and what criteria, tests, and diagnostics are required.
We were all born once, and we will all eventually leave this world. Just as we care deeply about the conditions under which a child is born—we have maternity hospitals, prenatal care, and an entire system—we must also care about the circumstances in which a person dies.
Ira: What advice would you give to colleagues in other countries with limited resources who are also striving to develop palliative care amid shortages of staff, knowledge, and medicines?
Taalaigul: Of course, you always have to ‘look in your wallet.’
I dream of establishing a fully functioning hospice. However, I also recognise that before progressing to advanced palliative care, we first need to ensure we have the essentials.
Taalaigul with colleagues / Personal photo archive
The WHO offers an excellent guide on integrating palliative care into primary health care, which we refer to regularly. It clearly states: even if resources are limited, a minimum level of care must be guaranteed—for example, morphine tablets or laxatives. That is the fundamental level, and it must be accessible. The government is obliged to subsidise it. You may lack oxygen concentrators or inpatient facilities, but you can organise care at home. We did the maths; one home visit costs far less than hospitalisation. Therefore, we need to develop mobile care systems. These don't necessarily require a doctor; a properly trained nurse or medical assistant can manage them. They must know how to deliver basic care, assess pain, and use simple diagnostic tools.
The palliative system should be organised as a clear patient pathway. It starts with the family doctor and nurse, who recognise when the patient is in pain or experiencing serious symptoms. If they are able to assist—excellent. If some procedures cannot be done at home, the patient can be temporarily transferred to a district hospital, and the family can be guided on how to provide care at home. If the patient needs a specialist consultation, an online appointment can be arranged with a palliative care doctor. And if specialised intervention is required—for example, radiation therapy—the patient is referred to a tertiary hospital. The main point is that people shouldn’t fall through the gaps between primary care and hospitals. There needs to be a clear pathway, not a series of barriers.
Ira: Which organisations, structures, or professionals act as role models or sources of support, inspiration, and professional strength for you?
Taalaigul: When it comes to people who have been guiding lights for me in palliative care, I would definitely name Olga Mychko from Belarus first. She serves as a personal example to me, a true mentor, even if she doesn’t realise it. I visited her in Minsk, accompanied her doctors on home visits, and studied all the documents and protocols for how palliative care is provided in Belarus.
I genuinely admire how clearly, concisely, and systematically things are organised there. It’s a remarkable structure. I paid particular attention to adult palliative care, and they’ve truly developed it with great care and understanding.
Another significant example for me is Professor Odontuya from Mongolia. She speaks Russian, studied in St. Petersburg (when it was still Leningrad), then in Poland, and later worked in the United States. She’s not just a doctor, she’s someone who is reforming her country’s healthcare system. And she’s doing it calmly, methodically, and convincingly. She came to Kyrgyzstan and gave lectures—a person who truly lives and breathes palliative care, a real leader, and a source of inspiration.
Of course, there’s Stephen Connor—my personal point of reference. Calm, gentle, thoughtful, yet someone with significant influence. Every encounter with him is worth noting and revisiting again and again.
Nyuta Federmesser. Few people can speak, articulate, persuade, and build a team quite like she does. She’s charismatic, precise, and a true leader. I admire her style, her approach, and her energy.
I am also very familiar with the work of the Vera Foundation in Russia. I have never visited them personally, but I read their website, follow their activities, and frequently use the materials they translate, especially the books on the fundamentals of palliative care. It provides real, practical help and is of very high quality.
Sechenov University is currently hosting excellent webinars. You can sense the high level of professionalism there.
At one point, I studied the palliative care standards in Romania. They have a hospice in the city of Brașov that serves as a very good example. Everything is systematic and carefully planned.
Once, I was in Kazakhstan for unrelated matters to palliative care, but I requested to visit the Palliative Care Centre in Almaty. They have 100 beds, with one nurse for every 10 beds, all as it should be. They gave me a tour, showed me around, and I found their example very inspiring.
But honestly, I’m motivated by anything that truly works and makes a difference. I’m always reading guidelines, articles, and newsletters. I observe how palliative care develops in India and Ukraine. I browse simply to stay informed. I don’t aim to study everything in detail, but it provides me with a solid foundation.
The palliative system should be organised as a clear patient pathway. It starts with the family doctor and nurse, who recognise when the patient is in pain or experiencing serious symptoms. If they are able to assist—excellent. If some procedures cannot be done at home, the patient can be temporarily transferred to a district hospital, and the family can be guided on how to provide care at home. If the patient needs a specialist consultation, an online appointment can be arranged with a palliative care doctor. And if specialised intervention is required—for example, radiation therapy—the patient is referred to a tertiary hospital. The main point is that people shouldn’t fall through the gaps between primary care and hospitals. There needs to be a clear pathway, not a series of barriers.
Ira: Which organisations, structures, or professionals act as role models or sources of support, inspiration, and professional strength for you?
Taalaigul: When it comes to people who have been guiding lights for me in palliative care, I would definitely name Olga Mychko from Belarus first. She serves as a personal example to me, a true mentor, even if she doesn’t realise it. I visited her in Minsk, accompanied her doctors on home visits, and studied all the documents and protocols for how palliative care is provided in Belarus.
I genuinely admire how clearly, concisely, and systematically things are organised there. It’s a remarkable structure. I paid particular attention to adult palliative care, and they’ve truly developed it with great care and understanding.
Another significant example for me is Professor Odontuya from Mongolia. She speaks Russian, studied in St. Petersburg (when it was still Leningrad), then in Poland, and later worked in the United States. She’s not just a doctor, she’s someone who is reforming her country’s healthcare system. And she’s doing it calmly, methodically, and convincingly. She came to Kyrgyzstan and gave lectures—a person who truly lives and breathes palliative care, a real leader, and a source of inspiration.
Of course, there’s Stephen Connor—my personal point of reference. Calm, gentle, thoughtful, yet someone with significant influence. Every encounter with him is worth noting and revisiting again and again.
Nyuta Federmesser. Few people can speak, articulate, persuade, and build a team quite like she does. She’s charismatic, precise, and a true leader. I admire her style, her approach, and her energy.
I am also very familiar with the work of the Vera Foundation in Russia. I have never visited them personally, but I read their website, follow their activities, and frequently use the materials they translate, especially the books on the fundamentals of palliative care. It provides real, practical help and is of very high quality.
Sechenov University is currently hosting excellent webinars. You can sense the high level of professionalism there.
At one point, I studied the palliative care standards in Romania. They have a hospice in the city of Brașov that serves as a very good example. Everything is systematic and carefully planned.
Once, I was in Kazakhstan for unrelated matters to palliative care, but I requested to visit the Palliative Care Centre in Almaty. They have 100 beds, with one nurse for every 10 beds, all as it should be. They gave me a tour, showed me around, and I found their example very inspiring.
But honestly, I’m motivated by anything that truly works and makes a difference. I’m always reading guidelines, articles, and newsletters. I observe how palliative care develops in India and Ukraine. I browse simply to stay informed. I don’t aim to study everything in detail, but it provides me with a solid foundation.
Whenever I’m beginning something new or encountering a challenge, I tell myself: ‘Stop. Let’s look at the guidelines first.’ That’s my approach.
Ira: How do you find allies—people and organisations who become your partners, support you, provide information and resources, and help open doors?
Taalaigul: That requires a lot of effort. We organise meetings, give talks, write, speak to people, and try to persuade them. The Soros Foundation did a great deal, especially in the early years. They were able to send people on internships, exchanges, and site visits, which was incredibly helpful because when someone sees how things operate in another country, they become motivated. They start to envisage what’s possible.
It’s important to develop personal, trusting relationships with government institutions. As a non-governmental organisation, of course, we can be critical, but we also need to find common ground, offer constructive criticism, and present facts rather than merely complaints. Milana says: ‘Research is power.’ And I completely agree. If you conduct good research, with solid data and figures, it’s difficult to argue against that. That’s why we believe in research. We think you should gather facts, analyse them, and use that evidence to build strong arguments and influence change.
Taalaigul: That requires a lot of effort. We organise meetings, give talks, write, speak to people, and try to persuade them. The Soros Foundation did a great deal, especially in the early years. They were able to send people on internships, exchanges, and site visits, which was incredibly helpful because when someone sees how things operate in another country, they become motivated. They start to envisage what’s possible.
It’s important to develop personal, trusting relationships with government institutions. As a non-governmental organisation, of course, we can be critical, but we also need to find common ground, offer constructive criticism, and present facts rather than merely complaints. Milana says: ‘Research is power.’ And I completely agree. If you conduct good research, with solid data and figures, it’s difficult to argue against that. That’s why we believe in research. We think you should gather facts, analyse them, and use that evidence to build strong arguments and influence change.
Palliative care leaders often stress the importance of research and data in developing structured palliative care systems. More on the power of evidence in PACED’s interview with Martin Loučka, founder of the Centre for Palliative Care in Prague, Czech Republic.
Ira: How can someone in Kyrgyzstan today develop a professional and educational pathway to become a palliative care specialist?
Taalaigul: The first thing that comes to mind is sending someone for training in Moscow, to one of the hospices run by the Vera Foundation, so they can observe what it should look like in practice. Here in Kyrgyzstan, the only place where you can truly learn is in oncology, because that’s where doctors are best equipped.
I can give you an example. We fought for a long time to establish a separate palliative care hospital, a hospice. Eventually, we were allotted a good facility, but it wasn't specifically for palliative care; instead, it was designated as a rehabilitation centre for stroke patients. Now, we’re trying to get everything up and running. However, the doctors there aren’t trained. We immediately told them to study at the National Oncology Centre, and we will also provide training ourselves. My next thought was: we need to find funding to send people for internships in Moscow so they can see and understand how everything operates: management, medical procedures, and the whole system.
We sent specialists to train with Olga Viktorovna in Minsk whenever we had the opportunity.
Taalaigul: The first thing that comes to mind is sending someone for training in Moscow, to one of the hospices run by the Vera Foundation, so they can observe what it should look like in practice. Here in Kyrgyzstan, the only place where you can truly learn is in oncology, because that’s where doctors are best equipped.
I can give you an example. We fought for a long time to establish a separate palliative care hospital, a hospice. Eventually, we were allotted a good facility, but it wasn't specifically for palliative care; instead, it was designated as a rehabilitation centre for stroke patients. Now, we’re trying to get everything up and running. However, the doctors there aren’t trained. We immediately told them to study at the National Oncology Centre, and we will also provide training ourselves. My next thought was: we need to find funding to send people for internships in Moscow so they can see and understand how everything operates: management, medical procedures, and the whole system.
We sent specialists to train with Olga Viktorovna in Minsk whenever we had the opportunity.
Practice, immersion, and hands-on experience are the most essential and practical parts of developing a palliative care specialist.
I also really like the format of online case consultations. It would be great if our doctors participated not just as listeners, but also delivered presentations themselves. Because when you present something, you become more engaged. Having cross-country case discussions like that would be very beneficial. We truly need a platform like this. It’s vital to stay informed about what’s happening with our neighbours, not just in distant countries, but right here in the region. We read each other’s news, exchange practices, and that’s what genuinely propels us forward.
Ira: Taalaigul, I have a brief, rapid-fire section left—five quick questions, just ‘question–answer.’
Your real-life heroes or heroines?
Taalaigul: Honestly, I don’t build heroes for myself; I walk my own path. But I do admire people who dedicate themselves to meaningful work and live their lives with dignity.
Ira: Are you afraid of death?
Taalaigul: Death—no. Sometimes I ask myself, ‘If I were to die today, am I ready?’ And I answer: ‘Yes, I’m ready.’ The only thing I wouldn’t want is suffering.
Ira: What do you believe constitutes strength?
Taalaigul: Faith is strength. It provides you with inner stability, purpose, and direction. That could be faith in God, or in kindness, humanity, or in people. I believe I would be deeply unhappy if I lacked faith.
Ira: Which ability would you like to possess?
Taalaigul: Oh, I know this one for sure. I’d love to have a good memory. Memory and mental clarity—those are wonderful gifts.
Ira: What is your most cherished dream?
Taalaigul: That there would be no more wars, no more suffering. That people would understand how fragile and small our planet is.
One time, my husband and I were discussing this, and he showed me a photo of Earth taken from a great distance by a satellite. In the image, our planet appears as merely a tiny dot. Yet here we are, still fighting, hurting one another, causing pain. I want people to realise how vital it is to protect what we have, to help each other, and to be kinder.
Your real-life heroes or heroines?
Taalaigul: Honestly, I don’t build heroes for myself; I walk my own path. But I do admire people who dedicate themselves to meaningful work and live their lives with dignity.
Ira: Are you afraid of death?
Taalaigul: Death—no. Sometimes I ask myself, ‘If I were to die today, am I ready?’ And I answer: ‘Yes, I’m ready.’ The only thing I wouldn’t want is suffering.
Ira: What do you believe constitutes strength?
Taalaigul: Faith is strength. It provides you with inner stability, purpose, and direction. That could be faith in God, or in kindness, humanity, or in people. I believe I would be deeply unhappy if I lacked faith.
Ira: Which ability would you like to possess?
Taalaigul: Oh, I know this one for sure. I’d love to have a good memory. Memory and mental clarity—those are wonderful gifts.
Ira: What is your most cherished dream?
Taalaigul: That there would be no more wars, no more suffering. That people would understand how fragile and small our planet is.
One time, my husband and I were discussing this, and he showed me a photo of Earth taken from a great distance by a satellite. In the image, our planet appears as merely a tiny dot. Yet here we are, still fighting, hurting one another, causing pain. I want people to realise how vital it is to protect what we have, to help each other, and to be kinder.
Changemakers

