Odontuya Davaasuren is a Doctor of Medical Sciences, a physician, an educator, and a key figure in the history of palliative care in Mongolia. For over 25 years, she has dedicated herself to advancing the field: training doctors and nurses, collaborating with government institutions, translating and publishing WHO materials, building a professional community, and advocating for palliative care to be recognised not as charity, but as an essential part of the national healthcare system.
In a new interview for the Changemakers series, Professor Odontuya speaks with Katerina from PACED about Mongolia—a country of striking contrasts and vast distances—her journey into medicine, the personal losses that steered her towards palliative care, and how the determination of one individual can instigate systemic change across an entire nation.
Читать текст на Русском
In a new interview for the Changemakers series, Professor Odontuya speaks with Katerina from PACED about Mongolia—a country of striking contrasts and vast distances—her journey into medicine, the personal losses that steered her towards palliative care, and how the determination of one individual can instigate systemic change across an entire nation.
Читать текст на Русском
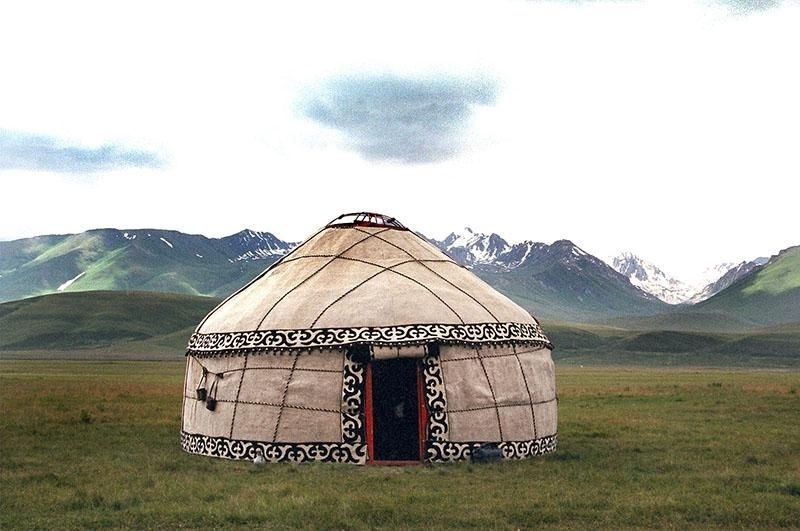
Yurts
A portable, cone-shaped shelter traditionally used by nomadic peoples of Asia.
Thyrotoxicosis
is a clinical syndrome that occurs when there is an excessive level of thyroid hormones in the blood.
An autoimmune disorder.
Now known as St. Petersburg State Paediatric Medical University.
From the 1920s to the 1980s, the Mongolian People’s Republic was greatly influenced by the USSR and adopted numerous Soviet political and administrative practices, including the state-mandated assignment of university graduates to workplaces.
Approximately 25 euro cents.
Obliterative endarteritis is a chronic arterial disease, most commonly affecting the arteries of the lower limbs, where the vessel lumen narrows or becomes completely blocked.
Nyam-Osor Nyamdorj
Minister of Health of Mongolia from 2000 to 2004.

Natsagiin Udval
Mongolian public official who served as Vice Minister of Health in the early 2000s. She later became the Minister of Health of Mongolia and led several national reforms in public health.

Jan Stjernswärd
a Swedish oncologist and palliative care specialist who served as an international consultant to the World Health Organisation (WHO) on palliative care.
Dogsomyn Tuya
Member of the State Great Khural and Minister of Health of Mongolia from 2004 to 2008.
Dr. Altankhuyag
Director of Ulaanbaatar's first hospice—Hope Hospice.
Katerina: Could you tell our readers a little about Mongolia?
Odontuya: Mongolia is a vast country, covering over 1.5 million square kilometres, but it has a small population of just over 3.5 million people. More than half of the population lives in the capital, Ulaanbaatar. The city comprises nine districts, each with its own district hospital. Across the country, Mongolia has 21 aimags (provinces), and the distances between them can be pretty long. For example, this summer, my family and I left Ulaanbaatar at seven in the morning. We didn't reach Arkhangai aimag until ten in the evening—and that’s not even that far.
Mongolia also possesses vast natural resources, such as gold, coal, uranium, and more. Sadly, foreign companies control a significant portion of extraction rights, including Chinese, Canadian, and others. They purchase licences to develop deposits, and in my opinion, this is not the proper approach.
There are many medical institutes and universities in Mongolia. Unfortunately, due to low salaries, many Mongolian professionals leave the country to work abroad. I read that around thirty thousand Mongolians go overseas for work each year. Often, they move to South Korea, where wages for the same job can be dozens or even hundreds of times higher. Those who speak English and other languages tend to migrate to Western countries.
Another significant issue is the environment. On the outskirts of Ulaanbaatar, many private homes still rely on coal for heating, which causes severe smog in the city. For years, the government has discussed the need to improve the environmental situation, but in reality, the air remains heavily polluted, especially during winter.
Odontuya: Mongolia is a vast country, covering over 1.5 million square kilometres, but it has a small population of just over 3.5 million people. More than half of the population lives in the capital, Ulaanbaatar. The city comprises nine districts, each with its own district hospital. Across the country, Mongolia has 21 aimags (provinces), and the distances between them can be pretty long. For example, this summer, my family and I left Ulaanbaatar at seven in the morning. We didn't reach Arkhangai aimag until ten in the evening—and that’s not even that far.
Mongolia also possesses vast natural resources, such as gold, coal, uranium, and more. Sadly, foreign companies control a significant portion of extraction rights, including Chinese, Canadian, and others. They purchase licences to develop deposits, and in my opinion, this is not the proper approach.
There are many medical institutes and universities in Mongolia. Unfortunately, due to low salaries, many Mongolian professionals leave the country to work abroad. I read that around thirty thousand Mongolians go overseas for work each year. Often, they move to South Korea, where wages for the same job can be dozens or even hundreds of times higher. Those who speak English and other languages tend to migrate to Western countries.
Another significant issue is the environment. On the outskirts of Ulaanbaatar, many private homes still rely on coal for heating, which causes severe smog in the city. For years, the government has discussed the need to improve the environmental situation, but in reality, the air remains heavily polluted, especially during winter.
Mongolia is a land of contrasts.
In Ulaanbaatar, you can see modern glass high-rises and newly developed neighbourhoods, while in rural areas, people still live in yurts and mainly depend on livestock herding. Winters are cold, and summers are very hot. Cities experience traffic congestion, whereas in villages, the main modes of transport are horses or camels. To the north lies the taiga; in the centre, extensive steppes; and in the south, deserts. We also have Lake Khövsgöl—a large, clean, crystal-clear freshwater lake, almost resembling a sea. From one shore, the other is not visible. Around Khövsgöl, reindeer herders live in small wooden shelters.
Katerina: How did you become a doctor? And how has your career progressed?
Odontuya: My journey into medicine started in childhood. When I was twelve, my mother passed away. She had thyrotoxicosis—Graves’ disease. She lost a lot of weight and suffered from tachycardia. Twice, doctors scheduled surgery to remove her thyroid gland, but the anaesthetists were hesitant to administer anaesthesia because she had heart disease and arrhythmia. The operation was delayed repeatedly, and ultimately, my mother died from a condition that is, in fact, treatable.
When I was twelve, in my fifth year of school, I made a firm decision to become a doctor. I remember writing in a school essay titled 'Who I Want to Be': ‘I want to become a doctor. I don’t want people to die. I don’t want children to live without parents.’
I entered the medical school through a competitive process. I had excellent grades and chose the Leningrad Paediatric Medical Institute, from which I graduated with honours. My first speciality is paediatrics.
During my first year of studies, my father passed away. He had lung cancer. At that time, flights were very expensive, so we travelled by train—the journey from Ulaanbaatar to Leningrad took five days. My father was dying in May, during my exam period, and my sister decided not to tell me so I could focus on my exams. In the summer, I returned home, and instead of my father meeting me at the station, my sisters were waiting for me. I remember entering the house and seeing his portrait on the wall with a black ribbon. It was a terrible shock. I felt physically ill—I couldn’t eat or drink; everything inside me shut down. I never had the chance to say goodbye or kiss him one last time.
When I later learnt how much he had suffered, it became even more difficult. He experienced severe shortness of breath and chest pain. My sister was studying medicine in Ulaanbaatar at the time and was caring for him. My father was a chemistry professor at the university, a highly respected man; his students helped as much as they could, but he still endured great suffering before his death.
Katerina: How did you become a doctor? And how has your career progressed?
Odontuya: My journey into medicine started in childhood. When I was twelve, my mother passed away. She had thyrotoxicosis—Graves’ disease. She lost a lot of weight and suffered from tachycardia. Twice, doctors scheduled surgery to remove her thyroid gland, but the anaesthetists were hesitant to administer anaesthesia because she had heart disease and arrhythmia. The operation was delayed repeatedly, and ultimately, my mother died from a condition that is, in fact, treatable.
When I was twelve, in my fifth year of school, I made a firm decision to become a doctor. I remember writing in a school essay titled 'Who I Want to Be': ‘I want to become a doctor. I don’t want people to die. I don’t want children to live without parents.’
I entered the medical school through a competitive process. I had excellent grades and chose the Leningrad Paediatric Medical Institute, from which I graduated with honours. My first speciality is paediatrics.
During my first year of studies, my father passed away. He had lung cancer. At that time, flights were very expensive, so we travelled by train—the journey from Ulaanbaatar to Leningrad took five days. My father was dying in May, during my exam period, and my sister decided not to tell me so I could focus on my exams. In the summer, I returned home, and instead of my father meeting me at the station, my sisters were waiting for me. I remember entering the house and seeing his portrait on the wall with a black ribbon. It was a terrible shock. I felt physically ill—I couldn’t eat or drink; everything inside me shut down. I never had the chance to say goodbye or kiss him one last time.
When I later learnt how much he had suffered, it became even more difficult. He experienced severe shortness of breath and chest pain. My sister was studying medicine in Ulaanbaatar at the time and was caring for him. My father was a chemistry professor at the university, a highly respected man; his students helped as much as they could, but he still endured great suffering before his death.
I returned to Leningrad. My classmates knew that my father had died, but I felt awkward and ashamed—I couldn’t talk to anyone about it. It was a closed, heavy experience.
After graduating, I was assigned to the medical institute in Ulaanbaatar to teach at the Department of Paediatrics. At that time, it was the only higher medical education institution in the country; today, it is the Mongolian National University of Medical Sciences. I taught there and, at the same time, worked as a doctor at the Maternal and Child Health Centre—without pay. I worked this way for around fifteen years.
In the late 1990s, family medicine started to develop in Mongolia. In 1998, I was offered the role of Head of the Department of General Medicine at my institute. I felt very anxious—it was a completely new field. But the director insisted, and I took the position. The department comprised specialists from various disciplines: a paediatrician, a physician, an obstetrician-gynaecologist, and a surgeon. I had to relearn almost everything from the beginning: the fundamentals of internal medicine, surgery, obstetrics and gynaecology, and psychiatry.
In the late 1990s, family medicine started to develop in Mongolia. In 1998, I was offered the role of Head of the Department of General Medicine at my institute. I felt very anxious—it was a completely new field. But the director insisted, and I took the position. The department comprised specialists from various disciplines: a paediatrician, a physician, an obstetrician-gynaecologist, and a surgeon. I had to relearn almost everything from the beginning: the fundamentals of internal medicine, surgery, obstetrics and gynaecology, and psychiatry.
In Mongolia, we say: ‘The wealthiest person is the one who possesses knowledge.’
That was when I truly felt it. I studied tirelessly, and my knowledge expanded, allowing me to help children, adults, and individuals with mental health issues, cancer, and chronic illnesses. Today, I work in two clinics and see patients of various ages facing different challenges. I have genuinely become wealthy—and this wealth will stay with me for the rest of my life.
Katerina: How did you start in palliative care?
Odontuya: When I first took on the role of leading the Department of General Practice, I travelled to Poland for a training programme funded by the Soros Foundation—a five-day course focusing on surgical and palliative medicine. That was the first time I ever encountered the term palliative medicine. During my student years in the 1980s, no one talked about palliative care at all.
The training was highly challenging for me: I barely knew English. I understood almost nothing, but I jotted everything down. I returned home with a suitcase full of materials. At that time, I didn’t have a computer, let alone the internet, so I sat with a dictionary and a pencil, translating every word and writing Mongolian translations in the margins. Sometimes I visited internet cafés, printed materials sent to me upon request, and spent nights translating them.
It was the early 2000s. That was when I first learned about the philosophy of palliative care — about how to support people when their illness is incurable.
Shortly after I had just graduated and started working in the department, my mother-in-law fell ill. She lived in the Arkhangai region and came to Ulaanbaatar with a severely swollen abdomen—she had ascites and liver cancer. I cared for her at home while also looking after my infant daughter. At that time, maternity leave in Mongolia lasted only 45 days after childbirth, so I was working, breastfeeding, and caring for a dying woman all at once. She died in my arms.
After completing that course, I realised that palliative care was precisely what had been missing back then. People like my mother-in-law, like my father, and like thousands and hundreds of thousands of others, deserve relief from suffering, care, and support until the end of life.
After returning home from the training, I began to consider my next steps. Should I implement Western methods, or first understand what people in Mongolia genuinely need? I decided to start small. At that time, I had two family medicine residents—young doctors.
Katerina: How did you start in palliative care?
Odontuya: When I first took on the role of leading the Department of General Practice, I travelled to Poland for a training programme funded by the Soros Foundation—a five-day course focusing on surgical and palliative medicine. That was the first time I ever encountered the term palliative medicine. During my student years in the 1980s, no one talked about palliative care at all.
The training was highly challenging for me: I barely knew English. I understood almost nothing, but I jotted everything down. I returned home with a suitcase full of materials. At that time, I didn’t have a computer, let alone the internet, so I sat with a dictionary and a pencil, translating every word and writing Mongolian translations in the margins. Sometimes I visited internet cafés, printed materials sent to me upon request, and spent nights translating them.
It was the early 2000s. That was when I first learned about the philosophy of palliative care — about how to support people when their illness is incurable.
Shortly after I had just graduated and started working in the department, my mother-in-law fell ill. She lived in the Arkhangai region and came to Ulaanbaatar with a severely swollen abdomen—she had ascites and liver cancer. I cared for her at home while also looking after my infant daughter. At that time, maternity leave in Mongolia lasted only 45 days after childbirth, so I was working, breastfeeding, and caring for a dying woman all at once. She died in my arms.
After completing that course, I realised that palliative care was precisely what had been missing back then. People like my mother-in-law, like my father, and like thousands and hundreds of thousands of others, deserve relief from suffering, care, and support until the end of life.
After returning home from the training, I began to consider my next steps. Should I implement Western methods, or first understand what people in Mongolia genuinely need? I decided to start small. At that time, I had two family medicine residents—young doctors.
We visited family physicians and asked them for the addresses of seriously ill, bedbound patients. I borrowed a video camera from a friend—I didn’t own one—and we went to these homes to observe how people lived and what their needs were.
Одонтуяа Даваасурэн / Фото PACED
In winter, it is often dark in Mongolia. We did this on weekends—leaving before sunrise, visiting the addresses provided by family doctors. We spoke with patients, their relatives, and carers, recording everything on video. We returned home after dark. In the evenings, I played the tapes, sat in front of the TV, and watched everything we had filmed that day.
The stories were different. For example, an elderly couple: the wife had cancer, and her husband was caring for her. They survived solely on a pension, which was not even enough to buy a litre of milk. The woman could no longer eat and could not tolerate the smell of meat. The husband said, ‘She asks for milk, but I don’t even have money for that.’ At the time, a litre of milk cost 500 tugriks.
There was a 38-year-old man with obliterating endarteritis. He had both of his legs amputated. He described it as feeling like hundreds of needles were piercing his amputated limbs—the pain was unbearable. Once, he got prescribed ten ampoules of morphine, which lasted for two days. When he returned asking for more, he was refused: by law, it was permitted only once. He told us that he had tried to take his own life twice because he could no longer endure the pain. I still have the cassette with his interview on it.
We met an older woman being cared for by her daughter. To earn some money, the daughter sewed on an old machine while her mother slept. I remember her saying, ‘I don’t know how to go on. I am a single mother, I pay for my son’s education, I care for my mother, and I’ve been unemployed for two years. I don’t know how we will survive.’
I watched these recordings repeatedly and reached several significant conclusions.
First: Mongolia desperately needs palliative care.
Second: Every family—anywhere in the world, regardless of income—will, sooner or later, face a situation in which someone close needs palliative support. It is inevitable: if a person is born, they will eventually die. It is fortunate if it happens quickly and without pain, but that is not always the case.
Third: Access to pain relief, especially morphine, must be ensured. Ten ampoules for two days is not adequate care—it is cruelty.
Fourth: Palliative care is not just about medicine; it also involves social support. Families caring for a bedridden person often live in poverty and require assistance not only from doctors but also from social services—including financial aid and care.
Fifth: Palliative care is not just for cancer patients. People with chronic, neurological, vascular, and age-related conditions also need care, support, and pain relief.
The stories were different. For example, an elderly couple: the wife had cancer, and her husband was caring for her. They survived solely on a pension, which was not even enough to buy a litre of milk. The woman could no longer eat and could not tolerate the smell of meat. The husband said, ‘She asks for milk, but I don’t even have money for that.’ At the time, a litre of milk cost 500 tugriks.
There was a 38-year-old man with obliterating endarteritis. He had both of his legs amputated. He described it as feeling like hundreds of needles were piercing his amputated limbs—the pain was unbearable. Once, he got prescribed ten ampoules of morphine, which lasted for two days. When he returned asking for more, he was refused: by law, it was permitted only once. He told us that he had tried to take his own life twice because he could no longer endure the pain. I still have the cassette with his interview on it.
We met an older woman being cared for by her daughter. To earn some money, the daughter sewed on an old machine while her mother slept. I remember her saying, ‘I don’t know how to go on. I am a single mother, I pay for my son’s education, I care for my mother, and I’ve been unemployed for two years. I don’t know how we will survive.’
I watched these recordings repeatedly and reached several significant conclusions.
First: Mongolia desperately needs palliative care.
Second: Every family—anywhere in the world, regardless of income—will, sooner or later, face a situation in which someone close needs palliative support. It is inevitable: if a person is born, they will eventually die. It is fortunate if it happens quickly and without pain, but that is not always the case.
Third: Access to pain relief, especially morphine, must be ensured. Ten ampoules for two days is not adequate care—it is cruelty.
Fourth: Palliative care is not just about medicine; it also involves social support. Families caring for a bedridden person often live in poverty and require assistance not only from doctors but also from social services—including financial aid and care.
Fifth: Palliative care is not just for cancer patients. People with chronic, neurological, vascular, and age-related conditions also need care, support, and pain relief.
Two days of filming profoundly changed my life. I received no grants and did not write any projects—I simply did what I felt was necessary. I wanted these videos to be watched by everyone, so that no one could ever say again: ‘We don’t have such patients.’ They exist. They suffer. And they need help.
That is how I started in palliative care.
Katerina: What was your following action?
Odontuya: I went to the Ministry of Health with a strong belief that Mongolia needed palliative care. At that time, the Minister was Mr N. Nyamdorj, and the Vice Minister was Ms N. Udval. I went directly to see the Minister, but he told me that palliative medicine was the responsibility of charitable organisations, not the Ministry of Health. Hearing this was very upsetting, but it did not deter me. Around the same time, I saw an announcement about a grant from the Soros Foundation. I barely knew English then, but I decided to try anyway. With a dictionary, literally translating each word, I drafted a project proposal to develop a basic educational programme in palliative medicine for doctors and medical university faculty, as well as to translate key World Health Organisation materials into Mongolian.
We are speaking of the early 2000s. I still remember writing that proposal by hand, with a dictionary, lots of mistakes, and pencil notes. A month later, I received a response: the project was approved. I could hardly believe it.
With support from the Soros Foundation grant, we translated several key WHO documents into Mongolian and published them, including guidelines on pain management and the fundamentals of palliative care. Later, we published two more crucial books that we still rely on today:
That same year, I established the Mongolian Palliative Care Association. With backing from the Soros Foundation, I trained around 300 doctors and medical university lecturers in the fundamental principles of palliative medicine. I personally led these five-day courses, using materials I had brought back and translated. When you teach, you learn yourself. I immersed myself more deeply in the field, reading new materials, seeking out WHO publications, and learning from international practices.
Katerina: What was your following action?
Odontuya: I went to the Ministry of Health with a strong belief that Mongolia needed palliative care. At that time, the Minister was Mr N. Nyamdorj, and the Vice Minister was Ms N. Udval. I went directly to see the Minister, but he told me that palliative medicine was the responsibility of charitable organisations, not the Ministry of Health. Hearing this was very upsetting, but it did not deter me. Around the same time, I saw an announcement about a grant from the Soros Foundation. I barely knew English then, but I decided to try anyway. With a dictionary, literally translating each word, I drafted a project proposal to develop a basic educational programme in palliative medicine for doctors and medical university faculty, as well as to translate key World Health Organisation materials into Mongolian.
We are speaking of the early 2000s. I still remember writing that proposal by hand, with a dictionary, lots of mistakes, and pencil notes. A month later, I received a response: the project was approved. I could hardly believe it.
With support from the Soros Foundation grant, we translated several key WHO documents into Mongolian and published them, including guidelines on pain management and the fundamentals of palliative care. Later, we published two more crucial books that we still rely on today:
- ‘Ensuring Balance in National Policies on Controlled Substances: Guidance for the Availability and Accessibility of Controlled Medicines’ and
- ‘Achieving Balance in National Opioids Control Policy: Guidelines for Assessing Medical Needs for Opioid Analgesics’.
That same year, I established the Mongolian Palliative Care Association. With backing from the Soros Foundation, I trained around 300 doctors and medical university lecturers in the fundamental principles of palliative medicine. I personally led these five-day courses, using materials I had brought back and translated. When you teach, you learn yourself. I immersed myself more deeply in the field, reading new materials, seeking out WHO publications, and learning from international practices.
With each new cohort, my knowledge expanded, along with my confidence that palliative care must become a part of Mongolia’s healthcare system rather than remain a charitable initiative.
Одонтуяа Даваасурэн с коллегами / Фото PACED
I then authored another project—this time aimed at improving national palliative care policy—and once again, the Soros Foundation supported it. In 2002, I organised a two-day leadership conference on palliative care in Ulaanbaatar. I invited an international WHO consultant in palliative medicine, Jan Stjernswärd. Representatives from the Ministry of Health attended, including the Vice Minister, directors of all nine district health departments of the capital, and chief physicians from all regions of Mongolia. Even those living more than a thousand kilometres away attended at their own expense because they understood how important it was. I had no funds to cover their travel—the grant was small, about three thousand dollars, and only enough for organisation, venue rental, and publication of materials.
Those two days marked a turning point. I delivered a presentation quantifying the number of deaths in Mongolia each year, the limited support available, and what the final days look like. I compared Mongolia to Poland, noting that Mongolia—a vast country—had only one six-bed palliative unit at the oncology centre in Ulaanbaatar. In contrast, Poland, a much smaller nation, had a nationwide network of hospices for adults and children, as well as mobile services.
That single palliative care ward in Mongolia appeared at the initiative of the oncology centre director, with support from American donors. Neither the state nor the Ministry of Health contributed a single tugrik. Furthermore, for three consecutive years, the ward had no morphine at all—can you imagine? A palliative care unit without pain relief.
I distributed the WHO books we had translated on balancing opioid control policies to all participants. At the end of each book, there is a questionnaire for health policymakers with answers ‘Yes’, ‘No’, and ‘I don’t know’. I asked everyone to complete it during the conference. When they did, they saw for themselves how underdeveloped palliative care was in Mongolia.
Those two days marked a turning point. I delivered a presentation quantifying the number of deaths in Mongolia each year, the limited support available, and what the final days look like. I compared Mongolia to Poland, noting that Mongolia—a vast country—had only one six-bed palliative unit at the oncology centre in Ulaanbaatar. In contrast, Poland, a much smaller nation, had a nationwide network of hospices for adults and children, as well as mobile services.
That single palliative care ward in Mongolia appeared at the initiative of the oncology centre director, with support from American donors. Neither the state nor the Ministry of Health contributed a single tugrik. Furthermore, for three consecutive years, the ward had no morphine at all—can you imagine? A palliative care unit without pain relief.
I distributed the WHO books we had translated on balancing opioid control policies to all participants. At the end of each book, there is a questionnaire for health policymakers with answers ‘Yes’, ‘No’, and ‘I don’t know’. I asked everyone to complete it during the conference. When they did, they saw for themselves how underdeveloped palliative care was in Mongolia.
And then something I had dreamed of happened: policymakers and health leaders themselves began standing up and saying that Mongolia needed to organise palliative care—not only in Ulaanbaatar, but also in the aimags.
They spoke about cancer patients in their areas who had no pain relief and about provinces where morphine was completely unavailable.
I remember when Dr Stjernswärd reviewed Mongolia’s morphine consumption data and asked me, ‘How many kilograms of morphine does the country use annually?’ I replied, ‘About one kilogram’. He chuckled, thinking I was joking. The next day, after examining the data himself, he apologised.
Dr Stjernswärd also spoke at that conference—very powerfully. I have never been afraid to argue with anyone, even members of parliament. When you talk about the truth, there is nothing to fear. Jan Stjernswärd was the same: loud, emotional, sincere. He convinced officials that developing a state palliative care system was their responsibility to the people.
Vice Minister Udval was also present—a wise woman. After the conference, the Ministry of Health issued an order to establish a working group on organising palliative care in Mongolia. The group included leaders of medical universities to integrate palliative medicine into undergraduate and postgraduate education, as well as ministry officials responsible for medication and drug imports. Their task was to develop new regulations to change opioid prescribing rules. They also formed subgroups on education, clinical standards, and service organisation. Funding was limited, but the groups worked very actively.
I remember when Dr Stjernswärd reviewed Mongolia’s morphine consumption data and asked me, ‘How many kilograms of morphine does the country use annually?’ I replied, ‘About one kilogram’. He chuckled, thinking I was joking. The next day, after examining the data himself, he apologised.
Dr Stjernswärd also spoke at that conference—very powerfully. I have never been afraid to argue with anyone, even members of parliament. When you talk about the truth, there is nothing to fear. Jan Stjernswärd was the same: loud, emotional, sincere. He convinced officials that developing a state palliative care system was their responsibility to the people.
Vice Minister Udval was also present—a wise woman. After the conference, the Ministry of Health issued an order to establish a working group on organising palliative care in Mongolia. The group included leaders of medical universities to integrate palliative medicine into undergraduate and postgraduate education, as well as ministry officials responsible for medication and drug imports. Their task was to develop new regulations to change opioid prescribing rules. They also formed subgroups on education, clinical standards, and service organisation. Funding was limited, but the groups worked very actively.
By 2004, palliative medicine had been incorporated into the curricula of all medical universities in Mongolia—initially with a limited number of hours, but it marked a significant achievement.
The Mongolian Palliative Care Association, which I led, received official approval to offer postgraduate training in palliative medicine for doctors and nurses. At first, the courses lasted three months; later, we extended them to six months.
In the early years, I taught alone. Classes for doctors and nurses took place every evening from 6 to 9 pm. The course fee was just 12,000 tugriks—less than three US dollars. When the course expanded to six months, the cost rose to 30,000 tugriks, about ten dollars. We did everything we could to keep education affordable. The Soros Foundation no longer funded these courses; the association organised everything independently. I wrote and published the first palliative care textbooks in Mongolian. We sold them at a modest price, and the proceeds supported the association.
Since 2005, we have celebrated World Hospice and Palliative Care Day every year. I also personally raised funds for this—partly through book and course sales, and partly from pharmaceutical companies that assisted with conference organisation, publications, and venue rental.
I have led the Mongolian Palliative Care Association for 25 years and have never received an official salary. I worked—and still work—purely out of commitment. When I later found out, for example, that the head of the Family Medicine Association receives a monthly salary, I was surprised—I had never considered money. I did everything simply because I believed it was necessary.
Every year, we organise events for World Hospice and Palliative Care Day. Usually, we rent a hall at the Ministry of Health, which grants us a 50% discount. We deliver lectures, hold conferences, and invite students and doctors.
Katerina: How did your relationships with decision-makers in government develop over time? Were you able to maintain their interest in palliative care?
Odontuya: The hardest part is dealing with politicians. They attend a conference, sit through an hour, then leave, claiming they are busy. Yet, they are precisely the people you need to connect with—to reach their very hearts.
In the early years, I taught alone. Classes for doctors and nurses took place every evening from 6 to 9 pm. The course fee was just 12,000 tugriks—less than three US dollars. When the course expanded to six months, the cost rose to 30,000 tugriks, about ten dollars. We did everything we could to keep education affordable. The Soros Foundation no longer funded these courses; the association organised everything independently. I wrote and published the first palliative care textbooks in Mongolian. We sold them at a modest price, and the proceeds supported the association.
Since 2005, we have celebrated World Hospice and Palliative Care Day every year. I also personally raised funds for this—partly through book and course sales, and partly from pharmaceutical companies that assisted with conference organisation, publications, and venue rental.
I have led the Mongolian Palliative Care Association for 25 years and have never received an official salary. I worked—and still work—purely out of commitment. When I later found out, for example, that the head of the Family Medicine Association receives a monthly salary, I was surprised—I had never considered money. I did everything simply because I believed it was necessary.
Every year, we organise events for World Hospice and Palliative Care Day. Usually, we rent a hall at the Ministry of Health, which grants us a 50% discount. We deliver lectures, hold conferences, and invite students and doctors.
Katerina: How did your relationships with decision-makers in government develop over time? Were you able to maintain their interest in palliative care?
Odontuya: The hardest part is dealing with politicians. They attend a conference, sit through an hour, then leave, claiming they are busy. Yet, they are precisely the people you need to connect with—to reach their very hearts.
Одонтуяа Даваасурэн / Фото PACED
Changing politicians’ attitudes towards palliative care is what has turned my hair grey.
Teaching students is straightforward now. All my lectures are recorded and accessible on YouTube—I can simply share a link. Even as we speak, my students are watching three lectures: What Is Palliative Medicine, The Goals and Principles of Palliative Care, and How to Communicate Difficult Messages.
So lectures can now run mainly on their own. However, changing health policy remains the most challenging task—particularly when it involves opioid prescribing regulations.
In 2004, the Ministry of Health introduced a new regulation that allowed not only oncologists but also primary care doctors—family physicians—to prescribe morphine. However, the issue remained that morphine itself was still in very short supply. There was not enough even for cancer patients, and we are still addressing this problem today.
It is crucial to recognise that Ministers of Health change frequently. You work with one, persuade them, ‘rewire’ their thinking, and they start to understand and support you—then they are replaced. A new one steps in, and everything begins again. You explain it to the second, the third, the fourth. It is exhausting work because politicians are busy, often hard to reach, and shifting their mindset isexceptionallyy challenging.
In 2005, we organised another conference at the Ministry of Health, as we usually did in October for World Hospice and Palliative Care Day. At that time, the Minister of Health was D. Tuya, a wise and attentive woman. She told us that the following year, 2006, they would revise all major Mongolian laws: the Health Law, the Social Welfare Law, and the Health Insurance Law. She said this was our chance and that we needed to work actively to include palliative care in these new laws.
At our very first conference in 2002, I told politicians that they were violating the Mongolian Constitution. They were surprised—how so? I explained:
So lectures can now run mainly on their own. However, changing health policy remains the most challenging task—particularly when it involves opioid prescribing regulations.
In 2004, the Ministry of Health introduced a new regulation that allowed not only oncologists but also primary care doctors—family physicians—to prescribe morphine. However, the issue remained that morphine itself was still in very short supply. There was not enough even for cancer patients, and we are still addressing this problem today.
It is crucial to recognise that Ministers of Health change frequently. You work with one, persuade them, ‘rewire’ their thinking, and they start to understand and support you—then they are replaced. A new one steps in, and everything begins again. You explain it to the second, the third, the fourth. It is exhausting work because politicians are busy, often hard to reach, and shifting their mindset isexceptionallyy challenging.
In 2005, we organised another conference at the Ministry of Health, as we usually did in October for World Hospice and Palliative Care Day. At that time, the Minister of Health was D. Tuya, a wise and attentive woman. She told us that the following year, 2006, they would revise all major Mongolian laws: the Health Law, the Social Welfare Law, and the Health Insurance Law. She said this was our chance and that we needed to work actively to include palliative care in these new laws.
At our very first conference in 2002, I told politicians that they were violating the Mongolian Constitution. They were surprised—how so? I explained:
If we send an incurably ill patient home, we are denying them medical care. But they are still alive, still citizens of the country. And the Constitution clearly states that every citizen of Mongolia has the right to medical care.
It turned out those words had made an impression on Ms Tuyaa, and she supported us.
By that time, I had a computer, and together with my colleague and friend Altankhuyag, we started drafting letters to members of parliament.
Altankhuyag was then the secretary of the Mongolian Palliative Care Association and the director of the country’s first hospice—Hope Hospice—founded with the support of a Christian medical community. They initially provided home care and later opened a 10-bed inpatient facility.
We wrote the letters very carefully—clear and precise, but not demanding. First came polite words and appreciation for their work, and then, on half a page, precisely what needed to be changed in the law.
We prepared three different letters: one for the Health Law, one for the Health Insurance Law, and one for the Social Welfare Law. In each letter, we explicitly specified which article and paragraph needed amendments to include palliative care and to ensure state budget financing.
In the Health Law, we proposed adding a paragraph obligating the government to finance palliative care from the health budget. At that time, hospices and palliative centres existed only on charitable funding.
In the letter on health insurance, we argued that insurance funds should cover at least some of the costs of palliative care.
And in the letter on social welfare, we requested provisions ensuring financial support for families caring for severely ill patients.
We reviewed the laws ourselves—reading every paragraph carefully—to identify precisely the places to incorporate new provisions.
By that time, I had a computer, and together with my colleague and friend Altankhuyag, we started drafting letters to members of parliament.
Altankhuyag was then the secretary of the Mongolian Palliative Care Association and the director of the country’s first hospice—Hope Hospice—founded with the support of a Christian medical community. They initially provided home care and later opened a 10-bed inpatient facility.
We wrote the letters very carefully—clear and precise, but not demanding. First came polite words and appreciation for their work, and then, on half a page, precisely what needed to be changed in the law.
We prepared three different letters: one for the Health Law, one for the Health Insurance Law, and one for the Social Welfare Law. In each letter, we explicitly specified which article and paragraph needed amendments to include palliative care and to ensure state budget financing.
In the Health Law, we proposed adding a paragraph obligating the government to finance palliative care from the health budget. At that time, hospices and palliative centres existed only on charitable funding.
In the letter on health insurance, we argued that insurance funds should cover at least some of the costs of palliative care.
And in the letter on social welfare, we requested provisions ensuring financial support for families caring for severely ill patients.
We reviewed the laws ourselves—reading every paragraph carefully—to identify precisely the places to incorporate new provisions.
We did everything thoroughly: each large envelope contained two pages—one with thanks, the second with specific proposals. We understood that they wouldn’t read anything longer. The next day, Altankhuyag took a stack of these envelopes to parliament and personally handed them to every MP.
In 2006, we achieved a significant victory. For the first time, the term ‘palliative medicine’ was included in the Health Law. From that moment onwards, the state health budget began allocating funds for palliative care—initially only for 10 beds at the oncology centre—but it marked a historic milestone.
That same year, the new Social Welfare Law introduced a provision supporting families caring for seriously ill relatives. Initially, the support was very small—20,000 tugriks per month, about eight US dollars. Later, it increased to 80,000, and now it exceeds 200,000 tugriks—around 80 dollars per month. This money helps families buy nappies, care supplies, and food. It is modest, but for low-income families, it is a significant help.
For the first time, the state officially recognised that such people exist, that they need support, and that caring for them is not charity, but a responsibility of the system.
However, it soon became clear that the health budget was still minimal. It was barely sufficient. We then realised we also had to secure funding from the health insurance system, which had much greater resources. That took a lot of effort. We arranged meetings, argued, persuaded, made calls, and explained. I used to say:
That same year, the new Social Welfare Law introduced a provision supporting families caring for seriously ill relatives. Initially, the support was very small—20,000 tugriks per month, about eight US dollars. Later, it increased to 80,000, and now it exceeds 200,000 tugriks—around 80 dollars per month. This money helps families buy nappies, care supplies, and food. It is modest, but for low-income families, it is a significant help.
For the first time, the state officially recognised that such people exist, that they need support, and that caring for them is not charity, but a responsibility of the system.
However, it soon became clear that the health budget was still minimal. It was barely sufficient. We then realised we also had to secure funding from the health insurance system, which had much greater resources. That took a lot of effort. We arranged meetings, argued, persuaded, made calls, and explained. I used to say:
‘We need insurance not to treat a sore throat, but to protect us when we are most vulnerable’.
It wasn't until 2012 that health insurance officially began funding palliative care. That was a significant achievement.
Thus, palliative care ultimately became integrated into the system—not as charity, but as a part of public healthcare funded by both the state and insurance schemes.
After that, private clinics began to show interest in palliative care, as insurance coverage became available. Some asked me for advice; I visited, assisted, and explained. Many established palliative units and allocated beds, but quickly abandoned the idea—mortality rates increased, and for hospitals, this meant ‘bad statistics’.
In public hospitals, however, progress continued. Today, all 21 provinces in Mongolia have a palliative care unit, as does every district hospital in Ulaanbaatar. Each year, the Ministry of Health approves the number of beds, which influences funding—partly from the state budget and partly from insurance.
Thus, palliative care ultimately became integrated into the system—not as charity, but as a part of public healthcare funded by both the state and insurance schemes.
After that, private clinics began to show interest in palliative care, as insurance coverage became available. Some asked me for advice; I visited, assisted, and explained. Many established palliative units and allocated beds, but quickly abandoned the idea—mortality rates increased, and for hospitals, this meant ‘bad statistics’.
In public hospitals, however, progress continued. Today, all 21 provinces in Mongolia have a palliative care unit, as does every district hospital in Ulaanbaatar. Each year, the Ministry of Health approves the number of beds, which influences funding—partly from the state budget and partly from insurance.
There is now a Ministry of Health regulation requiring every provincial and district hospital to have at least three palliative care beds, with the requirement in place until 2027. Even prison hospitals now have three palliative beds each.
The oncology centre in Ulaanbaatar has 16 beds, and some large private hospitals have more than ten. Nationwide, there are over 220 palliative care beds, all financed through health insurance. We reached a milestone: palliative care is no longer charity, but part of the healthcare system.
Many hospices close precisely because charity alone is not sustainable. It is essential, but unstable. That is why I always tell colleagues from other countries: establish hospices with the support of foundations or religious organisations, but the most important thing is sustainability. Ensure palliative care is part of the state system—embedded in health law, insurance law, and the budget.
Education holds equal importance. Today in Mongolia, all 11 medical specialities—surgeons, anaesthesiologists, internists, TB specialists, and others—are required to complete a minimum of a 5-day introductory palliative care course as part of postgraduate training. I am very proud of that.
Department of Family Medicine at the National University of Medical Sciences provides postgraduate education. All faculty members there have completed the three-month palliative care course we developed and are now able to teach it at both undergraduate and postgraduate levels.
I personally teach undergraduate students in a 16-lecture course with 10 days of practical training. I also offer credit-based training for practising doctors.
What concerns me is that many young specialists do not speak English. I try to involve them in international organisations—for example, encouraging them to join the Asian Pacific Hospice Palliative Care Network (APHN). Membership costs only ten dollars a year, but even that can be too much for some, and without language skills, it becomes challenging.
Regrettably, many universities do not fully meet the standards for palliative care education. There is a shortage of teachers, funding, and time. That is why I am eager for the new generation not only to teach but also to engage with international organisations.
Katerina: What has provided you with emotional support all these years?
Odontuya: Probably the main thing supporting me is that people call me ‘the mother of palliative care in Mongolia’. A mother doesn’t abandon her children, does she? And I cannot leave this work either.
Of course, I am tired. However, it is important for me to train the next generation so that palliative care does not disappear when I am gone.
Over these twenty-five years, I have published more than one hundred books—if you include textbooks as well as conference proceedings.
Many hospices close precisely because charity alone is not sustainable. It is essential, but unstable. That is why I always tell colleagues from other countries: establish hospices with the support of foundations or religious organisations, but the most important thing is sustainability. Ensure palliative care is part of the state system—embedded in health law, insurance law, and the budget.
Education holds equal importance. Today in Mongolia, all 11 medical specialities—surgeons, anaesthesiologists, internists, TB specialists, and others—are required to complete a minimum of a 5-day introductory palliative care course as part of postgraduate training. I am very proud of that.
Department of Family Medicine at the National University of Medical Sciences provides postgraduate education. All faculty members there have completed the three-month palliative care course we developed and are now able to teach it at both undergraduate and postgraduate levels.
I personally teach undergraduate students in a 16-lecture course with 10 days of practical training. I also offer credit-based training for practising doctors.
What concerns me is that many young specialists do not speak English. I try to involve them in international organisations—for example, encouraging them to join the Asian Pacific Hospice Palliative Care Network (APHN). Membership costs only ten dollars a year, but even that can be too much for some, and without language skills, it becomes challenging.
Regrettably, many universities do not fully meet the standards for palliative care education. There is a shortage of teachers, funding, and time. That is why I am eager for the new generation not only to teach but also to engage with international organisations.
Katerina: What has provided you with emotional support all these years?
Odontuya: Probably the main thing supporting me is that people call me ‘the mother of palliative care in Mongolia’. A mother doesn’t abandon her children, does she? And I cannot leave this work either.
Of course, I am tired. However, it is important for me to train the next generation so that palliative care does not disappear when I am gone.
Over these twenty-five years, I have published more than one hundred books—if you include textbooks as well as conference proceedings.
I design every conference like a book: the first pages feature photographs and messages from the Minister of Health, members of parliament, and representatives of the WHO; then come our lectures and materials. It is not merely a report—it is advocacy for palliative care at the state level.
Одонтуяа Даваасурэн / Фото PACED
Katerina: We have a tradition: at the end of each interview, we conduct a quick lightning round—short questions and short answers.
Question 1
Which cultural aspect of Mongolia has most impacted your work in palliative care?
Odontuya: Mongolians are very family-oriented. This strong sense of responsibility for one’s family helped me immensely when working with politicians, because I could say that, sooner or later, their families would also need palliative care. They understood and agreed—because family is sacred to every Mongolian.
Question 2
What does death signify to you?
Odontuya: According to our national Buddhist belief, death is not an end but a rebirth. We see death as a journey, as movement, not as a final destination. I share this belief.
Question 3
And what does happiness mean to you?
Odontuya: Happiness is the quality of life. Quality of life means different things to different people, and everyone has their own idea of happiness.
For me, happiness is being with my family, my children and grandchildren.
When I was studying in San Diego, we received an assignment to write three pages about what we would do if we discovered we were terminally ill. Everyone wrote something different. I wrote the same sentence on all three pages: ‘I want to go home. I want to go home. I want to go home’.
Home is where my happiness lies. Now, my grandchildren are my sunshine and my joy.
Question 4
What is your favourite dish?
Odontuya: Just before this interview, I cooked a vegetable soup with rice for my grandchildren. I love vegetable soups—simple and light. And I love rice. But when I was a student in Leningrad, there were pastries with dried apricots sold near our institute—I absolutely loved them.
Question 1
Which cultural aspect of Mongolia has most impacted your work in palliative care?
Odontuya: Mongolians are very family-oriented. This strong sense of responsibility for one’s family helped me immensely when working with politicians, because I could say that, sooner or later, their families would also need palliative care. They understood and agreed—because family is sacred to every Mongolian.
Question 2
What does death signify to you?
Odontuya: According to our national Buddhist belief, death is not an end but a rebirth. We see death as a journey, as movement, not as a final destination. I share this belief.
Question 3
And what does happiness mean to you?
Odontuya: Happiness is the quality of life. Quality of life means different things to different people, and everyone has their own idea of happiness.
For me, happiness is being with my family, my children and grandchildren.
When I was studying in San Diego, we received an assignment to write three pages about what we would do if we discovered we were terminally ill. Everyone wrote something different. I wrote the same sentence on all three pages: ‘I want to go home. I want to go home. I want to go home’.
Home is where my happiness lies. Now, my grandchildren are my sunshine and my joy.
Question 4
What is your favourite dish?
Odontuya: Just before this interview, I cooked a vegetable soup with rice for my grandchildren. I love vegetable soups—simple and light. And I love rice. But when I was a student in Leningrad, there were pastries with dried apricots sold near our institute—I absolutely loved them.
CHANGEMAKERS

