Yakhyo Ziyaev / Foto by PACED
Yakhyo Ziyaev: We Plan to Develop Palliative and Hospice Care in Uzbekistan According to International Standards in the Next Four Years
Support from the state and the media, overcoming opioid fear and cultural nuances in communication with patients, cross-border humanism, and unwavering determination. Continuing the series of Changemakers interviews, Ira Chernozhukova, Programme Head at PACED, spoke with Dr. Yakhyo Ziyaev, an oncologist, Secretary-General of the Association of Oncologists of Uzbekistan, and one of the leaders of the palliative care movement in the country.
Вы можете прочитать интервью на русском языке по этой ссылке.
Вы можете прочитать интервью на русском языке по этой ссылке.
Andijan (Uzbek: Andijon
is a city in eastern Uzbekistan with a population of approximately 440,000.

Eric L Krakauer
M.D., Ph.D., Associate Professor of Medicine, Massachusetts General Hospital. Associate Professor of Global Health and Social Medicine, Harvard Medical School.

Rustam Narbaev
Head of the Children`s Hospice Taskin.
The cancer register
is an electronic database designed for the registration and record-keeping of patients with malignant neoplasms in regional institutions of Uzbekistan.
Gamma Knife
also known as the Leksell Gamma Knife, is a device used for stereotactic radiosurgery of brain pathologies.
CyberKnife
is a radiosurgical system designed for the treatment of benign and malignant tumours as well as other conditins.
Proton therapy
uses a high-energy proton beam to irradiate diseased tissue, most commonly in cancer treatment.
Tashkent (Uzbek: Toshkent)
the capital and largest city of Uzbekistan.
The Sechenov healthcare system
is an unofficial name of a budget-administrative model typical for post-Soviet countries. It implies centralized management of medical institutions, where each speciality has its own dedicated centre (e.g., oncology or cardiology centres). This system is inherited from Soviet times and is known for its high level of bureaucracy. The term originates from the name of Ivan Mikhailovich Sechenov, a renowned Russian physiologist, but it is not directly related to his work.
Kashkadarya Region (Uzbek: Qashqadaryo viloyati)
is located south of Uzbekistan.
Samarkand (Uzbek: Samarqand)
is the third most populous city in Uzbekistan and the administrative centre of the Samarkand Region.
Khorezm Region (Uzbek: Xorazm viloyati)
is located in the northwestern part of Uzbekistan. Its administrative center is the city of Urgench.
Fergana (Uzbek: Farg'ona)
is a major city in eastern Uzbekistan.
The Islamic Development Bank
is an international financial institution focused on financing economic and social development projects in the bank's member countries. It has 57 member states as shareholders, the largest of which is Saudi Arabia.
The United Nations Office for Project Services (UNOPS).
The United Nations Office for Project Services (UNOPS)
Управление ООН по обслуживанию проектов.
Public Health Model for Palliative Care Development. Source: Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the end of life [Internet]. Geneva: World Health Organization; 2014 [cited 2019 Jan 2]. Available from:
http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf.
http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf.

Gulnara Kunirova
is the President of the Kazakhstan Association for Palliative Care and the Executive Director of the public foundation United Against Cancer. Read the interview of the PACED team with Gulnara here :https://paced.org.uk/gulnara_eng

Taalaigul Sabyrbekova
Chair of the Public Foundation Ergene and Co-Chair of the Association for Palliative and Hospice Care of the Republic of Kyrgyzstan.

Diana Nevzorova
PhD in Medicine, director of the Clinical Centre at Sechenov First Moscow State Medical University, and chief external expert in palliative care at the Russian Ministry of Healthcare.

Stephen R. Connor
PhD – clinical health psychologist, palliative care consultant, and executive director of the Worldwide Hospice and Palliative Care Alliance (WHPCA).

Julie Ling
CEO of the European Association for Palliative Care, consultant technical officer for palliative care for the European Regional Office, Сhair of the World Hospice and Palliative Care Alliance.
Education in Palliative and End-of-Life Care (EPEC)
End-of-Life Nursing Education Consortium (ELNEC)
Dafna Kfir-Furman
an employee of the Embassy of Israel in Uzbekistan, was formerly a social worker at the oncology hospice of the Chaim Sheba Medical Centre, Israel's largest state medical centre.

Dr. Ron Sabar
is a specialist in palliative medicine and the founder of the palliative care service Sabar Clinics in Israel.
Elisabeth Kübler-Ross (1926–2004)
was an American psychologist of Swiss origin known for developing the concept of psychological support for terminally ill patients and her research on near-death experiences. She identified the five stages of grief: denial, anger, bargaining, depression, and acceptance.
The SPIKES protocol
designed for effective communication with seriously ill patients and their loved ones, consists of six steps: setting up, perception, invitation, knowledge, empathy, and strategy.
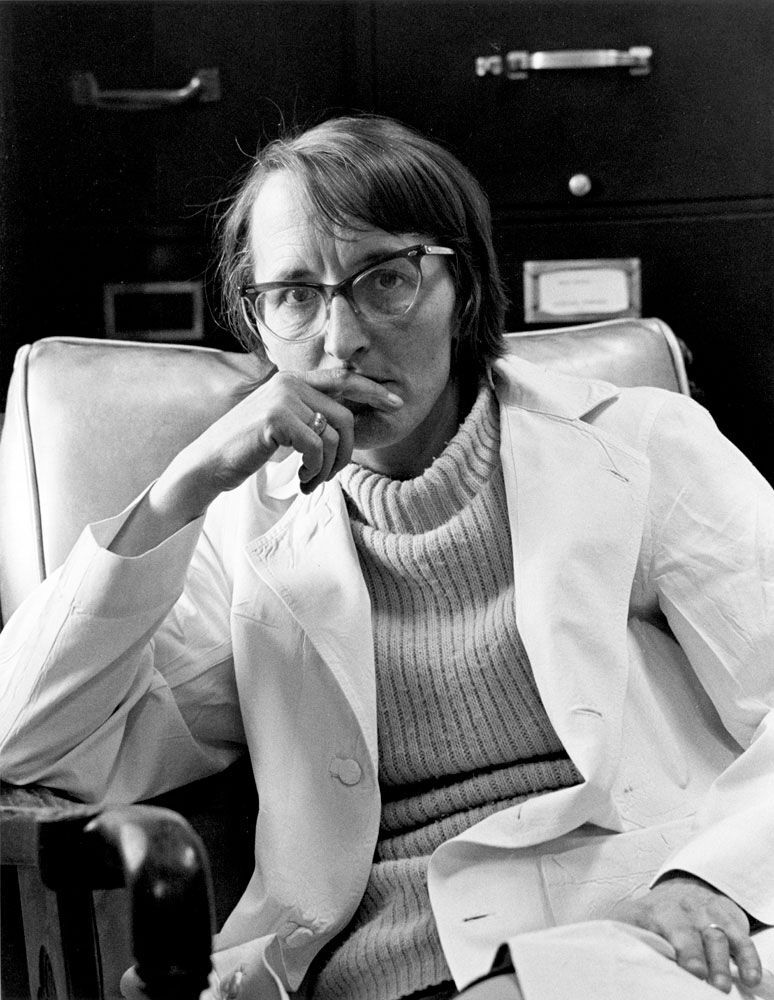
Ira: When did you develop a professional interest in end-of-life patient care?
Yakhyo: I am a hereditary oncologist, following in my father’s footsteps. My father also worked a lot, so workaholism runs in the family. I practically grew up at the Oncology Centre in Andijan. The nurses and orderlies there were like my second family. Oncology is what it is, and I often saw that at the end of a patient’s life, when there was nothing else to do, my father felt helpless. It troubled him greatly, and it troubled me along with him.
I realised that unless the fundamental question — how to help a terminally ill patient? — was solved, there was no point in discussing grander topics. The thought formed when I worked as a nurse between 2007 and 2010. I graduated in 2015, around the time of the first forum of oncology leaders of Central Asia, which Eric Krakauer attended. The stars aligned. He shared that palliative and hospice care development is a beautiful solution to this problem.
Yakhyo: I am a hereditary oncologist, following in my father’s footsteps. My father also worked a lot, so workaholism runs in the family. I practically grew up at the Oncology Centre in Andijan. The nurses and orderlies there were like my second family. Oncology is what it is, and I often saw that at the end of a patient’s life, when there was nothing else to do, my father felt helpless. It troubled him greatly, and it troubled me along with him.
I realised that unless the fundamental question — how to help a terminally ill patient? — was solved, there was no point in discussing grander topics. The thought formed when I worked as a nurse between 2007 and 2010. I graduated in 2015, around the time of the first forum of oncology leaders of Central Asia, which Eric Krakauer attended. The stars aligned. He shared that palliative and hospice care development is a beautiful solution to this problem.
We cannot cure everyone, but 'not being able to cure' does not mean 'not being able to help.'
I realised that this was my calling and that I needed to address the most fundamental oncology issue: palliative care. At that moment, in 2016, political changes were taking place: a new president, and the introduction of inclusivity at all levels in Uzbekistan — from society to ministries. We realised that we urgently needed palliative care. That’s how it all started and continued, up to the Cabinet of Ministers' resolution that guaranteed citizens access to palliative care as part of state-provided services.
My professional interest and decision to engage in palliative care took root in 2015. But even around 2010, I understood that the country needed such a service. In 2017, we started working with Rustam Narbaev, my former student who is now a colleague, and we gathered a team of like-minded people.
My professional interest and decision to engage in palliative care took root in 2015. But even around 2010, I understood that the country needed such a service. In 2017, we started working with Rustam Narbaev, my former student who is now a colleague, and we gathered a team of like-minded people.
Rustam Narbaev, Ira Chernozhukova, Yahyo Ziyaev / Photo by PACED
This year, we are launching the cancer register system, which is our brainchild. We decided to focus on developing areas with acute needs. Bringing and implementing a Gamma Knife, CyberKnife, or proton therapy in an unprepared infrastructure is not entirely rational, so we are moving in this direction.
Ira: You are fully involved in curing and accompanying patients at the end of life. Do these two approaches conflict?
Yakhyo: Undoubtedly, they do. But, as is known, palliative care starts with diagnosis. We have already established palliative care services within oncology — providing 200 palliative care beds across Uzbekistan, in all our branches, and here at the centre. I oversee this service. A new hospice is set to open in Tashkent soon, and we are eagerly anticipating it. I still see patients, but most of my time goes into addressing organisational matters. Still, establishing a hospice is not the same as creating a full-fledged palliative care structure.
We are working with the social protection agency to expand our services to other fields. Globally, oncology accounts for about 30% of palliative care, while the rest involves neurodegenerative diseases, gerontology, etc. But in Uzbekistan, it happened that oncologists began implementing this system. I understand this is not uncommon.
Ira: What is the current state of non-oncological palliative care in Uzbekistan?
Yakhyo: It’s lacking; it simply does not exist. Such patients are treated in specialised facilities, but when medical help is no longer possible, these clinics try to avoid admitting them. Unfortunately, patients are left alone with their pain, grief, and problems, which is troubling me.
Ira: You are fully involved in curing and accompanying patients at the end of life. Do these two approaches conflict?
Yakhyo: Undoubtedly, they do. But, as is known, palliative care starts with diagnosis. We have already established palliative care services within oncology — providing 200 palliative care beds across Uzbekistan, in all our branches, and here at the centre. I oversee this service. A new hospice is set to open in Tashkent soon, and we are eagerly anticipating it. I still see patients, but most of my time goes into addressing organisational matters. Still, establishing a hospice is not the same as creating a full-fledged palliative care structure.
We are working with the social protection agency to expand our services to other fields. Globally, oncology accounts for about 30% of palliative care, while the rest involves neurodegenerative diseases, gerontology, etc. But in Uzbekistan, it happened that oncologists began implementing this system. I understand this is not uncommon.
Ira: What is the current state of non-oncological palliative care in Uzbekistan?
Yakhyo: It’s lacking; it simply does not exist. Such patients are treated in specialised facilities, but when medical help is no longer possible, these clinics try to avoid admitting them. Unfortunately, patients are left alone with their pain, grief, and problems, which is troubling me.
I hope the new hospice in Tashkent will become a methodological centre for palliative and hospice care.
In Uzbekistan, the Sechenov health system is in place, a budget-administrative model where each speciality requires a separate institution, such as an oncology centre, cardiology centre, etc. The new hospice will serve as a centre for developing palliative and hospice care. Yes, we are starting with oncology, but we are looking forward. There is a development strategy for Uzbekistan until 2030, under which we set the goal for hospices to be present in all regions based on actual needs. There are only four hospices in Uzbekistan, five if you count the children’s hospice. So, we are starting with oncology because it’s urgent, but we do not plan to stop there. We will extend palliative care services to other areas.
Ira: In your opinion, what percentage of adult patients who need palliative care receive it?
Yakhyo: Approximately 10% to 20% of palliative patients receive high-quality palliative care, while the rest do not get enough of it. There are direct figures: the number of treated patients, the number of patients who have passed through palliative departments, and indirect indicators, such as "morphine consumption," meaning morphine use per capita in Uzbekistan. Worldwide, this figure is around 5 milligrams per capita, while in Uzbekistan, in 2020, it was 0.04 milligrams — catastrophically low. This means that people here die in pain, and that is partly our fault.
When the resolution on palliative care was issued in 2017, I didn’t yet have deep knowledge of its organisation. We thought establishing 50 beds in one region and creating an interregional department would be more efficient back then. Now, we understand that this is not the case. Uzbekistan is a large country, and travelling 200 km from Kashkadarya to Samarkand with a palliative or hospice patient is simply unreasonable. We acknowledge our mistake and plan to optimise and structure everything by 2030.
Ira: Could you tell us a bit about the hospices that already exist in Uzbekistan?
Yakhyo: A hospice was established in Khorezm in 2012. Initially, until 2018, it was more like a nursing home, but we reorganised it, trained the staff, and it began functioning as a full-fledged hospice. The Taskin Hospice appeared in 2022. The third hospice opened in Samarkand in 2023. The fourth and fifth hospices are in Fergana and Tashkent. They are in the final stages. We say they exist, but they are currently in the launch phase. They will start operating at the beginning of 2025. Everything is moving fast, but we wish it were even faster.
In 2022, Uzbekistan secured a large concessional loan from the Islamic Development Bank, including for the organisation and development of palliative care. Previously, such funds often got stuck somewhere, rarely reaching their intended purpose. But now everything is strictly monitored by international UN organisations: procurement through UNOPS and the development of palliative care in collaboration with WHO.
Ira: In your opinion, what percentage of adult patients who need palliative care receive it?
Yakhyo: Approximately 10% to 20% of palliative patients receive high-quality palliative care, while the rest do not get enough of it. There are direct figures: the number of treated patients, the number of patients who have passed through palliative departments, and indirect indicators, such as "morphine consumption," meaning morphine use per capita in Uzbekistan. Worldwide, this figure is around 5 milligrams per capita, while in Uzbekistan, in 2020, it was 0.04 milligrams — catastrophically low. This means that people here die in pain, and that is partly our fault.
When the resolution on palliative care was issued in 2017, I didn’t yet have deep knowledge of its organisation. We thought establishing 50 beds in one region and creating an interregional department would be more efficient back then. Now, we understand that this is not the case. Uzbekistan is a large country, and travelling 200 km from Kashkadarya to Samarkand with a palliative or hospice patient is simply unreasonable. We acknowledge our mistake and plan to optimise and structure everything by 2030.
Ira: Could you tell us a bit about the hospices that already exist in Uzbekistan?
Yakhyo: A hospice was established in Khorezm in 2012. Initially, until 2018, it was more like a nursing home, but we reorganised it, trained the staff, and it began functioning as a full-fledged hospice. The Taskin Hospice appeared in 2022. The third hospice opened in Samarkand in 2023. The fourth and fifth hospices are in Fergana and Tashkent. They are in the final stages. We say they exist, but they are currently in the launch phase. They will start operating at the beginning of 2025. Everything is moving fast, but we wish it were even faster.
In 2022, Uzbekistan secured a large concessional loan from the Islamic Development Bank, including for the organisation and development of palliative care. Previously, such funds often got stuck somewhere, rarely reaching their intended purpose. But now everything is strictly monitored by international UN organisations: procurement through UNOPS and the development of palliative care in collaboration with WHO.
We plan to develop palliative and hospice care in Uzbekistan according to international standards in the next four years.
Ira: How did you manage to launch such rapid development?
Yakhyo: First of all, the state changed. Do you remember the model for palliative care development? Access to medications and human resources, and overarching it all, like an umbrella, is political will. That is what worked initially. Previously, all attempts to develop palliative care ran into the narrative that our oncology is the best and no one dies of cancer here. Finally, the state stopped deceiving itself, and the Constitution was amended to enshrine that we are a socially oriented country where human dignity is central. Palliative and hospice care emphasise this more than anything else.
Yakhyo: First of all, the state changed. Do you remember the model for palliative care development? Access to medications and human resources, and overarching it all, like an umbrella, is political will. That is what worked initially. Previously, all attempts to develop palliative care ran into the narrative that our oncology is the best and no one dies of cancer here. Finally, the state stopped deceiving itself, and the Constitution was amended to enshrine that we are a socially oriented country where human dignity is central. Palliative and hospice care emphasise this more than anything else.
Secondly, people. We need people, specialists, and human capital. Everything has to come from within; we need to understand that palliative care is necessary. That is what we have been moving toward for years.
Thirdly, when realisation comes, you need somewhere to draw information from. For Uzbekistan, this is an entirely new field, a new structure, a new philosophy, so to speak. This is where international partners, organisations, and international cooperation came to our aid. With their help, we understood how to develop correctly, where to move next, and what to do.\
Fourth — and I think this is the most important — is persistence. When you do something new, people resist it. Rustam and I went around collecting signatures. When the Cabinet of Ministers' resolution was being formed, I waited for the deputy minister in the parking lot to talk and get a signature; otherwise, it wouldn’t move forward.
When we opened Taskin, we encountered people of the old school who believed that we would turn children into addicts and pump them full of opioids. I told Rustam that the main thing is to show perseverance and that we would not leave until we achieved our goal. And if something didn’t work out, we would go to the media.
Thirdly, when realisation comes, you need somewhere to draw information from. For Uzbekistan, this is an entirely new field, a new structure, a new philosophy, so to speak. This is where international partners, organisations, and international cooperation came to our aid. With their help, we understood how to develop correctly, where to move next, and what to do.\
Fourth — and I think this is the most important — is persistence. When you do something new, people resist it. Rustam and I went around collecting signatures. When the Cabinet of Ministers' resolution was being formed, I waited for the deputy minister in the parking lot to talk and get a signature; otherwise, it wouldn’t move forward.
When we opened Taskin, we encountered people of the old school who believed that we would turn children into addicts and pump them full of opioids. I told Rustam that the main thing is to show perseverance and that we would not leave until we achieved our goal. And if something didn’t work out, we would go to the media.
Political will, people, international cooperation, and persistence are the four pillars on which we are building palliative care in Uzbekistan.
Ira: When will the Tashkent hospice open?
Yakhyo: That’s a good question! Everything is almost ready. If there’s no progress by December 1, we will go there with journalists and do a big report on the delay. But we were promised that the hospice would open in January next year. I hope a video conference will be held directly from the new hospice in early 2025.
We have big plans. With the support of international colleagues, we plan to make the Tashkent hospice an educational centre for palliative care specialists, not only in Uzbekistan but throughout Central Asia. We have already discussed this with Gulnara Kunirova and Taalaigul Sabyrbekova.
Ira: What is currently lacking in the education of specialists in medical universities in Uzbekistan, in your opinion?
Yakhyo: Unfortunately, a major issue is communication with patients. In our universities, students are taught that medicine is powerful, that we can always cure everyone, and that patients should never be told what their illness is. Even in our Taskin hospice, people come with stage four cancer, and no one has informed either the patient or their relatives that this is palliative care, that this is the end of life. They are shocked that they were never told anything before.
The second issue — specific to palliative and hospice care — is the intense opioid phobia that is present in many post-Soviet countries. We are very hesitant to prescribe opioid analgesics. If we do, we often do it incorrectly: there is no competence, no skills to titrate opioids properly, to prescribe them correctly, and to maintain the right dosage. Until this year, there was a limit on the issuance of opioids — no more than 21 ampoules per prescription, which was a nightmare because patients were always left without enough. Moreover, opioids are only issued in central clinics, so some patients have to travel long distances to get a prescription and pain relief.
Both of these components need to be integrated into the educational program. By the way, after an article in Gazeta in which I discussed this, some progress has been made. We are now revising the bioethics course that second-year medical students take, orienting it toward communication with patients.
Yakhyo: That’s a good question! Everything is almost ready. If there’s no progress by December 1, we will go there with journalists and do a big report on the delay. But we were promised that the hospice would open in January next year. I hope a video conference will be held directly from the new hospice in early 2025.
We have big plans. With the support of international colleagues, we plan to make the Tashkent hospice an educational centre for palliative care specialists, not only in Uzbekistan but throughout Central Asia. We have already discussed this with Gulnara Kunirova and Taalaigul Sabyrbekova.
Ira: What is currently lacking in the education of specialists in medical universities in Uzbekistan, in your opinion?
Yakhyo: Unfortunately, a major issue is communication with patients. In our universities, students are taught that medicine is powerful, that we can always cure everyone, and that patients should never be told what their illness is. Even in our Taskin hospice, people come with stage four cancer, and no one has informed either the patient or their relatives that this is palliative care, that this is the end of life. They are shocked that they were never told anything before.
The second issue — specific to palliative and hospice care — is the intense opioid phobia that is present in many post-Soviet countries. We are very hesitant to prescribe opioid analgesics. If we do, we often do it incorrectly: there is no competence, no skills to titrate opioids properly, to prescribe them correctly, and to maintain the right dosage. Until this year, there was a limit on the issuance of opioids — no more than 21 ampoules per prescription, which was a nightmare because patients were always left without enough. Moreover, opioids are only issued in central clinics, so some patients have to travel long distances to get a prescription and pain relief.
Both of these components need to be integrated into the educational program. By the way, after an article in Gazeta in which I discussed this, some progress has been made. We are now revising the bioethics course that second-year medical students take, orienting it toward communication with patients.
All high-tech skills can be learned over time, and we can send our specialists abroad for training. But if there is no foundation or understanding of the essence of palliative care, what technology can we even talk about?
Ira: Do you plan to create a dedicated course or specialty in palliative care at a medical institution?
Yakhyo: We have already opened a department of oncology and palliative medicine. In the future, it will be based at the new hospice in Tashkent, but for now, it is at the city oncology branch.
We are also preparing a package of documents to include palliative care in the Health Law of the Republic of Uzbekistan. The law has not been revised on a large scale since 1999, but it is now in the plans, and we want palliative care to be listed there as one of the components of medical care. Right after that, we must include palliative care specialists and palliative care nurses in the professional registry at the Ministry of Labor. All this is planned for 2025. Moreover, we want to give these specialists — doctors and nurses — a status equivalent to resuscitation specialists because their emotional workload, if not more significant, is certainly not less.
Ira: Whose support has helped you influence such significant processes, and how did you secure that support?
Yakhyo: Unfortunately or fortunately, over the last 9 years, we have had nine health ministers. But we have public support. This month, we had a week of awareness in the field of palliative and hospice care. All TV channels dedicated prime-time slots to palliative care issues for an entire week. A week later, we reinforced this with a radio appearance. The media supports us, and influential people in society do as well.
Here’s a simple example. Previously, I didn’t know many legislative details, as I’m a doctor. A department head at the Ministry of Justice called me, saying he had read about us in the media, that his family had also been touched by palliative care, that he felt this pain, and that he wanted to help us. The department then reviewed the legislative framework for us, pointed out where there were problems and what we were missing, set deadlines, and helped us work in the right direction.
Parliament also supported the initiative. They gathered mayors and representatives from the Ministry of Health for a roundtable to discuss ways to develop palliative care in Uzbekistan.
Yakhyo: We have already opened a department of oncology and palliative medicine. In the future, it will be based at the new hospice in Tashkent, but for now, it is at the city oncology branch.
We are also preparing a package of documents to include palliative care in the Health Law of the Republic of Uzbekistan. The law has not been revised on a large scale since 1999, but it is now in the plans, and we want palliative care to be listed there as one of the components of medical care. Right after that, we must include palliative care specialists and palliative care nurses in the professional registry at the Ministry of Labor. All this is planned for 2025. Moreover, we want to give these specialists — doctors and nurses — a status equivalent to resuscitation specialists because their emotional workload, if not more significant, is certainly not less.
Ira: Whose support has helped you influence such significant processes, and how did you secure that support?
Yakhyo: Unfortunately or fortunately, over the last 9 years, we have had nine health ministers. But we have public support. This month, we had a week of awareness in the field of palliative and hospice care. All TV channels dedicated prime-time slots to palliative care issues for an entire week. A week later, we reinforced this with a radio appearance. The media supports us, and influential people in society do as well.
Here’s a simple example. Previously, I didn’t know many legislative details, as I’m a doctor. A department head at the Ministry of Justice called me, saying he had read about us in the media, that his family had also been touched by palliative care, that he felt this pain, and that he wanted to help us. The department then reviewed the legislative framework for us, pointed out where there were problems and what we were missing, set deadlines, and helped us work in the right direction.
Parliament also supported the initiative. They gathered mayors and representatives from the Ministry of Health for a roundtable to discuss ways to develop palliative care in Uzbekistan.
To summarise, society supports us, and that is a tremendous strength and a significant achievement for us.
Hospice Taskin / Foto by PACED
Ira: Which organisations and palliative care specialists do you look up to on your path?
Yakhyo: Of course, IAHPC and WHPCA, as well as the Palliative Care Association, particularly Diana Vladimirovna Nevzorova. Also, Fundacja Hospicyjna — a hospice oncology foundation in Poland — has greatly impressed me. As for specialists: Diana Vladimirovna, Eric Krakauer, Stephen Connor, Julie Ling, Gulnara Kunirova, Taalaigul Sabyrbekova, and Andrzej Ryś from Poland — dedicated individuals who not only develop palliative care in their own countries but also contribute significantly to its advancement worldwide.
Ira: You have learned from specialists from international organisations and aim for global standards. Both you and your colleagues, the people you train, are carriers of Western-style methods that do not always align with Uzbekistan's cultural code and traditions. Do you feel points of tension? How do you adapt work methods to the practice of your country and the people of Uzbekistan?
Yakhyo: Humanism is, after all, cross-border — humanism is humanism, whether in the USA, Israel, or Uzbekistan. You are right; I learned what I later applied to create the Taskin Children's Hospice at St. Jude Clinic in the United States through the EPEC and ELNEC programs.
When opening Taskin, we were assisted by wonderful Israeli partners — Dafna Kfir-Furman and Ron Sabar — with whom we conducted three-level training for our specialists.
Yakhyo: Of course, IAHPC and WHPCA, as well as the Palliative Care Association, particularly Diana Vladimirovna Nevzorova. Also, Fundacja Hospicyjna — a hospice oncology foundation in Poland — has greatly impressed me. As for specialists: Diana Vladimirovna, Eric Krakauer, Stephen Connor, Julie Ling, Gulnara Kunirova, Taalaigul Sabyrbekova, and Andrzej Ryś from Poland — dedicated individuals who not only develop palliative care in their own countries but also contribute significantly to its advancement worldwide.
Ira: You have learned from specialists from international organisations and aim for global standards. Both you and your colleagues, the people you train, are carriers of Western-style methods that do not always align with Uzbekistan's cultural code and traditions. Do you feel points of tension? How do you adapt work methods to the practice of your country and the people of Uzbekistan?
Yakhyo: Humanism is, after all, cross-border — humanism is humanism, whether in the USA, Israel, or Uzbekistan. You are right; I learned what I later applied to create the Taskin Children's Hospice at St. Jude Clinic in the United States through the EPEC and ELNEC programs.
When opening Taskin, we were assisted by wonderful Israeli partners — Dafna Kfir-Furman and Ron Sabar — with whom we conducted three-level training for our specialists.
Personalized office in honor of Daphne Kfir-Furman / Foto by PACED
We did not encounter much resistance from patients. On the contrary, they appreciate that we engage with them more. However, colleagues and patients' relatives are resistant.
For example, when I am about to go in and tell a patient that they have incurable cancer, their relatives won’t let me. Why? Because they think it will upset or anger them. But that’s a normal reaction! I have to talk to the family and explain the stages of grief according to Kübler-Ross.
The same is true for some colleagues. They think the patient isn’t ready. They fear the patient will commit suicide or file a lawsuit. I understand some of their fears: there have been cases where patients committed suicide, but it wasn’t because they were informed about their illness but because they were told there was no way to help.
There are different techniques for delivering such news. We usually follow the SPIKES protocol — we do not start serious conversations until we are sure the patient is ready, their relatives, environment, and even we, as doctors, are ready. This ensures the conversation is as comfortable for the patient as possible. Thus, the fears of suicide are unfounded.
For example, when I am about to go in and tell a patient that they have incurable cancer, their relatives won’t let me. Why? Because they think it will upset or anger them. But that’s a normal reaction! I have to talk to the family and explain the stages of grief according to Kübler-Ross.
The same is true for some colleagues. They think the patient isn’t ready. They fear the patient will commit suicide or file a lawsuit. I understand some of their fears: there have been cases where patients committed suicide, but it wasn’t because they were informed about their illness but because they were told there was no way to help.
There are different techniques for delivering such news. We usually follow the SPIKES protocol — we do not start serious conversations until we are sure the patient is ready, their relatives, environment, and even we, as doctors, are ready. This ensures the conversation is as comfortable for the patient as possible. Thus, the fears of suicide are unfounded.
Most of the time, when my patient says they don’t want to live, it’s not because they want to die but because they fear pain and being left alone with their illness.
People are becoming more aware of palliative care. The paradigm is slowly changing for patients and medical staff because the world is globalising. In the era of the open internet, whether we like it or not, many things will become homogenised.
However, it’s important to note that we do not tell patients bad news if they don’t want to know. Some feel more comfortable not knowing the truth and living in the moment. I fully support them. But such cases are rare. Usually, what happens? There’s a big metaphorical elephant in the room where the sick person lives. The patient knows the elephant is there, the relatives see it there, and the medical staff understands it, but no one talks about it. That’s an unhealthy situation! So, when we come and say “elephant,” just acknowledging its presence, communication between the patient and their family, and between the family and the medical staff, immediately improves.
However, it’s important to note that we do not tell patients bad news if they don’t want to know. Some feel more comfortable not knowing the truth and living in the moment. I fully support them. But such cases are rare. Usually, what happens? There’s a big metaphorical elephant in the room where the sick person lives. The patient knows the elephant is there, the relatives see it there, and the medical staff understands it, but no one talks about it. That’s an unhealthy situation! So, when we come and say “elephant,” just acknowledging its presence, communication between the patient and their family, and between the family and the medical staff, immediately improves.
Changmakers