In previous webinars of the pain management series, PACED experts discussed how to identify and assess pain. Now, we delve into how to treat it. Modern medicine offers a variety of effective methods for pain management, with opioid analgesics playing a central role in this process. This is a summary of a webinar on how to select opioid therapy for patients suffering from severe pain properly. Dr Narine Movsesyan from Armenia explained how to use opioids effectively and safely, outlined the challenges faced by specialists in pain management, and shared basic knowledge about the nature and properties of opioid analgesics, as well as the principles of opioid therapy.
We are pleased to introduce Narine Movsesyan, an anesthesiologist, Yerevan State Medical Institute lecturer, palliative care and pain management specialist, and an international leader in the Palliative Care Leadership Development Initiative, Cohort II, Yerevan.
You can watch the webinar recording in Russian or English on our YouTube channel.
Текст на русском языке.
We are pleased to introduce Narine Movsesyan, an anesthesiologist, Yerevan State Medical Institute lecturer, palliative care and pain management specialist, and an international leader in the Palliative Care Leadership Development Initiative, Cohort II, Yerevan.
You can watch the webinar recording in Russian or English on our YouTube channel.
Текст на русском языке.
“
Please be advised that the webinar is intended for palliative care specialists and medical professionals and contains information about prescribing pain medications in Armenia. Before applying the knowledge gained, we strongly recommend verifying it against the laws of the country where you practice regarding the use of narcotic drugs.
Contents
The History of Opioids
Pharmacodynamics of Opioids
Pharmacokinetics of Opioids
Consequences of Opioid Use
Classification of Opioids by Affinity for μ-Receptors
Patient Management Algorithms for Pain
Classification of Pain
Pain Intensity Assessment
Non-Opioid Analgesics
Principles of Using Opioid Analgesics
Principles of Prescribing Opioid Analgesics
Main Opioid Analgesics
Opioid Rotation
Opioid Antagonist Naloxone
Q&A Session
Question 1: Obstacles to Opioid Pain Management
Question 2: Conversation With Patients and Relatives About Opioid Analgesics
Question 3: What to Do if a Patient Refuses to Take Opioids
Question 4: What to Do if a Patient Cannot Assess Their Pain
Question 5: Patient-Controlled Anaesthesia
Pharmacodynamics of Opioids
Pharmacokinetics of Opioids
Consequences of Opioid Use
Classification of Opioids by Affinity for μ-Receptors
Patient Management Algorithms for Pain
Classification of Pain
Pain Intensity Assessment
Non-Opioid Analgesics
Principles of Using Opioid Analgesics
Principles of Prescribing Opioid Analgesics
Main Opioid Analgesics
Opioid Rotation
Opioid Antagonist Naloxone
Q&A Session
Question 1: Obstacles to Opioid Pain Management
Question 2: Conversation With Patients and Relatives About Opioid Analgesics
Question 3: What to Do if a Patient Refuses to Take Opioids
Question 4: What to Do if a Patient Cannot Assess Their Pain
Question 5: Patient-Controlled Anaesthesia
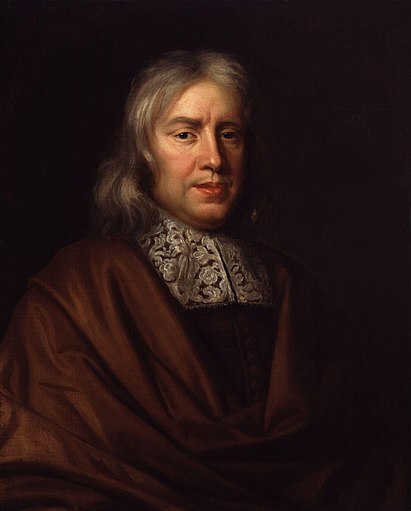
Thomas Sydenham
(1624–1689), a renowned English physician and reformer of clinical medicine in 17th-century England.

Friedrich Sertuerner
(1783–1841) a German pharmacist
The simultaneous invention by French surgeon Charles Pravaz and Scottish physician Alexander Wood.
The History of Opioids
Let’s take a brief historical look to understand where opioids came from. Scientists found the earliest opium prescriptions on clay tablets dating back around 8,000 years. Archaeological excavations have uncovered a pill containing opium dating back to 5,000 BCE. All ancient civilisations knew of opium, made opium tinctures, and used it as a panacea for all ailments. We can find references to opium in the Odyssey and the Bible. Notable figures such as Homer, George Franklin, and Napoleon were known to have used opium.
The use of alkaloids began with Thomas Sydenham in the 1660s. He created the mixture Laudanum — a blend of opium, saffron, cinnamon, and cloves in wine. Similar mixtures with varying concentrations of opium began appearing on the pharmaceutical market. Pure morphine was isolated from the opium poppy by the German pharmacologist Friedrich Sertürner in 1804. He named the substance morphium (morphine) after Morpheus, the Greek god of dreams. Morphine gained widespread popularity after the invention of the hypodermic needle in 1853 and was used for pain relief.
The use of alkaloids began with Thomas Sydenham in the 1660s. He created the mixture Laudanum — a blend of opium, saffron, cinnamon, and cloves in wine. Similar mixtures with varying concentrations of opium began appearing on the pharmaceutical market. Pure morphine was isolated from the opium poppy by the German pharmacologist Friedrich Sertürner in 1804. He named the substance morphium (morphine) after Morpheus, the Greek god of dreams. Morphine gained widespread popularity after the invention of the hypodermic needle in 1853 and was used for pain relief.
Pharmacodynamics of Opioids
How do opioids work?
Opioids act through three main types of opioid receptors:
Opioid receptors coupled with G-proteins (G-protein-coupled receptors, GPCRs) act as secondary messengers, activating a complex cascade of reactions that result in the analgesic process. These reactions include increased conductance through K+ channels, leading to the hyperpolarisation of sensory neurons.
The binding of opioid receptors leads to decreased conductance through calcium channels, reducing the release of neurotransmitters (such as glutamate) involved in nociception.
Finally, the binding of opioid receptors inhibits adenylate cyclase. Collectively, all these actions contribute to the development of analgesia.
Opioids act through three main types of opioid receptors:
- μ-opioid receptors, responsible for analgesia, respiratory depression, euphoria, and suppression of gastrointestinal motility;
- k-opioid receptors and σ-receptors, which have similar effects, responsible for analgesia, dysphoria, psychotomimetic effects, miosis, and respiratory depression;
- δ-opioid receptors, which are responsible for analgesia.
Opioid receptors coupled with G-proteins (G-protein-coupled receptors, GPCRs) act as secondary messengers, activating a complex cascade of reactions that result in the analgesic process. These reactions include increased conductance through K+ channels, leading to the hyperpolarisation of sensory neurons.
The binding of opioid receptors leads to decreased conductance through calcium channels, reducing the release of neurotransmitters (such as glutamate) involved in nociception.
Finally, the binding of opioid receptors inhibits adenylate cyclase. Collectively, all these actions contribute to the development of analgesia.
What do opioid receptors look like?
As I mentioned, μ-receptors, coupled with G-proteins, are also known as seven transmembrane or serpentine receptors, forming a large family of transmembrane receptors.
As I mentioned, μ-receptors, coupled with G-proteins, are also known as seven transmembrane or serpentine receptors, forming a large family of transmembrane receptors.
μ-receptors / PACED Webinar
This means that part of these receptors is located inside the cell, while another part is outside the cell.
The most important receptor for inducing analgesia is the μ-receptor. Synthetic opioid development aims to target the μ-receptor while minimizing the impact on k- and δ-receptors, which are responsible for side effects.
The most important receptor for inducing analgesia is the μ-receptor. Synthetic opioid development aims to target the μ-receptor while minimizing the impact on k- and δ-receptors, which are responsible for side effects.
Pharmacokinetics of Opioids
Lipophilicity
Opioid absorption depends on their lipophilicity, which determines the time it takes to reach the maximum concentration of opioids in plasma.
The lipophilicity of fentanyl is 820 times greater than that of morphine/hydromorphone. For methadone, it is 115 times greater. This means they have a highly pronounced ability to bind to nerves and adipose tissues. Due to its lipophilicity, fentanyl penetrates subcutaneous adipose tissue, forming a depot that ensures a steady influx and consistent concentration level of fentanyl, which is why it is often used in patches.
Plasma proteins and fat solubility influence the drug's distribution in the vascular system. A high redistribution coefficient into adipose tissues rapidly decreases the drug's concentration in the bloodstream. At the same time, if the volume of circulating blood is reduced, the peak concentration occurs faster, and the time to reach the maximum concentration is shortened.
Oral morphine reaches its peak in 60 minutes, subcutaneous administration in 30 minutes, and intravenous administration in 6 to 10 minutes. The half-life of immediate-release oral morphine is four hours. Steady-state equilibrium is established after four to five half-lives, which takes about 16-20 hours. This means that after the first or second tablet of morphine or the first or second injection, we cannot judge whether the dose is adequate or whether it provides effective pain relief. We must wait at least 4-5 half-lives to reach the maximum concentration. I will further illustrate how this occurs and its significance in opioid pain management.
Indirect factors also include the amount of body fat and total body water content. If we have a cachectic patient who is not only cachectic due to a progressive illness, such as a tumour, but also has a reduced volume of circulating blood, then even a small dose of opioids will result in a high peak concentration in a short time. Consider it when working with elderly patients. In their case, the peak concentration of pain medications occurs significantly faster than in others.
Opioid absorption depends on their lipophilicity, which determines the time it takes to reach the maximum concentration of opioids in plasma.
The lipophilicity of fentanyl is 820 times greater than that of morphine/hydromorphone. For methadone, it is 115 times greater. This means they have a highly pronounced ability to bind to nerves and adipose tissues. Due to its lipophilicity, fentanyl penetrates subcutaneous adipose tissue, forming a depot that ensures a steady influx and consistent concentration level of fentanyl, which is why it is often used in patches.
Plasma proteins and fat solubility influence the drug's distribution in the vascular system. A high redistribution coefficient into adipose tissues rapidly decreases the drug's concentration in the bloodstream. At the same time, if the volume of circulating blood is reduced, the peak concentration occurs faster, and the time to reach the maximum concentration is shortened.
Oral morphine reaches its peak in 60 minutes, subcutaneous administration in 30 minutes, and intravenous administration in 6 to 10 minutes. The half-life of immediate-release oral morphine is four hours. Steady-state equilibrium is established after four to five half-lives, which takes about 16-20 hours. This means that after the first or second tablet of morphine or the first or second injection, we cannot judge whether the dose is adequate or whether it provides effective pain relief. We must wait at least 4-5 half-lives to reach the maximum concentration. I will further illustrate how this occurs and its significance in opioid pain management.
Indirect factors also include the amount of body fat and total body water content. If we have a cachectic patient who is not only cachectic due to a progressive illness, such as a tumour, but also has a reduced volume of circulating blood, then even a small dose of opioids will result in a high peak concentration in a short time. Consider it when working with elderly patients. In their case, the peak concentration of pain medications occurs significantly faster than in others.
Excretion of Opioids
Most opioids undergo glucuronidation and dealkylation in the liver and are excreted by the kidneys. In the liver, morphine metabolises into morphine-6-glucuronide, which is responsible for analgesia, drowsiness, nausea, and decreased gastrointestinal motility, and morphine-3-glucuronide, which contributes more to toxicity, myoclonus, and accumulation in the body, especially in cases of kidney disease. Additionally, the seizure threshold lowers.
Liver diseases naturally affect metabolism. Therefore, the dose should be reduced for patients with liver disease and decreased metabolic function. Old age and genetic factors also influence metabolism. Thus, a drug may work differently in one patient compared to another. Most opioids are excreted by the kidneys, except for methadone, which is excreted through the intestines.
We should give special attention to patients with chronic renal failure, where the half-life of morphine, in particular, can be prolonged by 2.5 to 7.5 times. If the half-life is 4 hours and the next dose of morphine is administered every 4 hours, for patients with renal failure, this period extends to nearly 10 hours or more. Sometimes, even a single dose per day is sufficient. It is important to remember this when prescribing opioids to patients with renal failure to avoid overdosing. Patients undergoing dialysis tolerate dialysable fentanyl better than morphine and codeine.
Most opioids undergo glucuronidation and dealkylation in the liver and are excreted by the kidneys. In the liver, morphine metabolises into morphine-6-glucuronide, which is responsible for analgesia, drowsiness, nausea, and decreased gastrointestinal motility, and morphine-3-glucuronide, which contributes more to toxicity, myoclonus, and accumulation in the body, especially in cases of kidney disease. Additionally, the seizure threshold lowers.
Liver diseases naturally affect metabolism. Therefore, the dose should be reduced for patients with liver disease and decreased metabolic function. Old age and genetic factors also influence metabolism. Thus, a drug may work differently in one patient compared to another. Most opioids are excreted by the kidneys, except for methadone, which is excreted through the intestines.
We should give special attention to patients with chronic renal failure, where the half-life of morphine, in particular, can be prolonged by 2.5 to 7.5 times. If the half-life is 4 hours and the next dose of morphine is administered every 4 hours, for patients with renal failure, this period extends to nearly 10 hours or more. Sometimes, even a single dose per day is sufficient. It is important to remember this when prescribing opioids to patients with renal failure to avoid overdosing. Patients undergoing dialysis tolerate dialysable fentanyl better than morphine and codeine.
Routes of Opioid Administration
- Oral (PO);
- Rectal;
- Intranasal;
- Buccal;
- Subcutaneous;
- Intravenous (IV, PCA);
- Transdermal (TD);
- Inhalational.
Consequences of Opioid Use
I am sure that everyone attending this webinar has some level of fear regarding opioids. Usually, this fear is greatly exaggerated, but we still need to understand the consequences of opioid use by patients.
Dependence
It is crucial to differentiate between different types of dependence:
Dependence
It is crucial to differentiate between different types of dependence:
- Physical dependence occurs when opioid intake suddenly stops or the dose sharply reduces. It is characterised by withdrawal syndrome and requires specific therapy. Withdrawal syndrome can lead to very undesirable reactions in the patient.
- Psychological dependence or addiction is marked by an irresistible psychological need for the opioid, loss of control over its consumption, and compulsive use despite the harm caused by the opioid.
- Pseudo-dependence is a mistaken belief in dependence in a patient who is seeking pain relief.
Tolerance
Tolerance refers to the desensitisation of opioid receptors, resulting in a gradual decrease in the therapeutic effect of the drug. It necessitates a gradual increase in the initially effective analgesic dose. For example, if effective pain relief was achieved with five milligrams every 4 hours, after a few days, the patient is likely to report that the pain has returned. Why? Because the opioid receptors have become less responsive to that dose, reducing both the duration and quality of analgesia. Therefore, we have to increase the dose of the drug.
Pseudo-tolerance is the incorrect belief that a dose increase is necessary due to developing tolerance, while poor analgesia is actually due to disease progression or other factors. Maintaining constant communication with the patient is essential to understand what is causing poor analgesia.
Tolerance refers to the desensitisation of opioid receptors, resulting in a gradual decrease in the therapeutic effect of the drug. It necessitates a gradual increase in the initially effective analgesic dose. For example, if effective pain relief was achieved with five milligrams every 4 hours, after a few days, the patient is likely to report that the pain has returned. Why? Because the opioid receptors have become less responsive to that dose, reducing both the duration and quality of analgesia. Therefore, we have to increase the dose of the drug.
Pseudo-tolerance is the incorrect belief that a dose increase is necessary due to developing tolerance, while poor analgesia is actually due to disease progression or other factors. Maintaining constant communication with the patient is essential to understand what is causing poor analgesia.
Classification of Opioids by Affinity for μ-Receptors
- Agonists;
- Partial agonists;
- Agonists/antagonists;
- Antagonists (the most well-known is Naloxone).
Patient Management Algorithms for Pain
- Determine whether we can eliminate the cause of the pain; sometimes, this is possible.
- Identify the type of pain: Nociceptive, Neuropathic, Mixed. The approach to treatment changes based on the type of pain. We treat nociceptive pain according to one set of protocols, neuropathic pain according to another, and mixed pain requires special attention and often involves not only nonsteroidal anti-inflammatory drugs or opioid analgesics but also other medications.
- Objectify the pain, i.e., assess its intensity. No matter how empathetic we are, we cannot feel someone else's pain, so we must evaluate it using a scale.
- Use both pharmacological and non-pharmacological treatments: pain management is an integrative process that includes all distraction methods and procedures that can alleviate pain.
- Take into account the individual characteristics of patients. Many patients have genetically determined features affecting how their opioid receptors interact with opioids. The same drug may work for one patient and not for another.
- Maintain feedback with the patient and monitor pain management. We always need to know if the treatment helped or not, whether to increase the dose, decrease it, or adjust it, and whether there are side effects. We cannot be one-time doctors. If we prescribe pain management, we must know how effective it is.
Classification of Pain
By Origin
- Nociceptive:
- Somatic;
- Visceral.
- Neuropathic;
- Idiopathic (psychogenic, psychosomatic, etc.).
By Duration
- Acute pain – has a predictable onset, course, and resolution. It stops as healing occurs and may last for hours, days, or weeks. If pain persists beyond the expected healing period, it is considered chronic.
- Chronic pain – pain that persists or recurs for more than 3 months, continues for 1 month after the resolution of acute tissue damage or is associated with non-healing injuries. It often has a wave-like or recurring nature, is accompanied by patient suffering, and reduces quality of life. Since 2022, according to the International Classification of Diseases 11th Revision (ICD-11), chronic pain has been defined as a separate diagnosis under code MG30.
Breakthrough Pain
Breakthrough pain is a temporary, sharp, spontaneous, or episodic exacerbation of pain that occurs despite the use of extended-release pain medications. It typically manifests as a sudden, intense, short-lived pain episode. It appears in 90% of cancer patients and 75% of non-cancer patients receiving opioids who are otherwise in a state of stable pain control.
Accidental or predictable breakthrough pain is associated with particular events, such as coughing, movement, dressing changes, etc. Unlike typical breakthrough pain, it is not spontaneous and can be anticipated.
Breakthrough pain is a temporary, sharp, spontaneous, or episodic exacerbation of pain that occurs despite the use of extended-release pain medications. It typically manifests as a sudden, intense, short-lived pain episode. It appears in 90% of cancer patients and 75% of non-cancer patients receiving opioids who are otherwise in a state of stable pain control.
Accidental or predictable breakthrough pain is associated with particular events, such as coughing, movement, dressing changes, etc. Unlike typical breakthrough pain, it is not spontaneous and can be anticipated.
Pain Intensity Assessment
Once we have identified that pain is present and determined it is chronic, the next step is assessing it. The gold standard for assessing pain intensity is the patient’s report. We use the visual analogue scale (VAS), a verbal scale, or, in exceptional cases, the Wong-Baker 'Faces' Pain Scale to evaluate pain objectively.
Wong-Baker Faces Pain Scale / Webinar PACED
In 1986, the World Health Organization (WHO) introduced the Pain Relief Ladder. It has three steps:
- Mild pain – managed with non-opioid analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), paracetamol, and adjuvants (1-3 on the VAS);
- Moderate pain – treated with weak opioids (4-6 on the VAS);
- Severe and unbearable pain – treated with solid opioids (6-10 on the VAS).
Webinar PACED
If a patient comes to you with pain that is objectively at the third step, there is no need to take them through all the levels of pain management; start with low doses of potent opioids.
Non-Opioid Analgesics
This category includes nonsteroidal anti-inflammatory drugs (NSAIDs) and paracetamol. We know that paracetamol has a less pronounced anti-inflammatory effect and is more of a good pain reliever. All NSAIDs have a limited prescription period — up to 10 days or 2-3 weeks — because of their significant impact on the gastrointestinal tract, the excretory system (particularly the kidneys), and platelets. Paracetamol can be prescribed for a more extended period, taking liver conditions, age, and other factors into account. There is no perfect scheme; we must use these drugs according to the patient and their characteristics.
It’s important to understand that the Pain Relief Ladder is not a rigid rule. Discussions are ongoing about removing the second step, as weak opioids are represented by tramadol and codeine. Codeine is metabolised into morphine and is not registered in some countries. Tramadol is not always effective and is 10 times weaker than morphine. Therefore, if there is significant pain and the means to control it, starting with low doses of morphine is a viable option. Instead of prescribing 50 mg of tramadol, 5 mg of morphine can be given, and the dose gradually increased.
It’s important to understand that the Pain Relief Ladder is not a rigid rule. Discussions are ongoing about removing the second step, as weak opioids are represented by tramadol and codeine. Codeine is metabolised into morphine and is not registered in some countries. Tramadol is not always effective and is 10 times weaker than morphine. Therefore, if there is significant pain and the means to control it, starting with low doses of morphine is a viable option. Instead of prescribing 50 mg of tramadol, 5 mg of morphine can be given, and the dose gradually increased.
Principles of Using Opioid Analgesics
- Oral Administration Whenever Possible. As in the joke, 'Patient, wake up. I need to give you a sleeping pill.' Why cause the patient additional pain when we can avoid it? This is applicable only to patients who can swallow.
- By the Clock. The patient should not experience pain. If the drug's half-life is 4 hours, the next dose should be administered after 4 hours. If it is 8 hours, then after 8 hours. We should not wait for the pain relief to wear off completely, as we would then have to start from scratch. Maintaining a consistent concentration of painkillers in the blood is essential.
- Individual Approach. Different genetic variations, side effects, and interactions must be considered. Lipophilicity and the amount of body water are also important. Therefore, we choose the drug individually and monitor the patient’s condition to determine the appropriate dosage.
- Attention to Details. I would call it feedback. We must understand that what works well today might not work tomorrow, or overdosing might occur. Continuous feedback, attention to detail, and monitoring for side effects should exist.
Principles of Prescribing Opioid Analgesics
It is essential to distinguish between patients who have never taken opioids and those who have already received them. A patient who has never taken an opioid analgesic is referred to as opioid-naive, which is an international term.
The starting doses for such opioid-naive patients should be minimal, followed by gradual increases. Suppose your patient was taking tramadol and is now transitioning to morphine. In that case, this patient is not considered opioid-naive, and the morphine dose can be calculated based on the tramadol dosage previously received. If the patient has no prior experience with opioids, you should start with the lowest dose and increase it as needed.
Opioid analgesic therapy should always start with 'pure' opioids rather than mixed formulations and always with short-acting drugs. Only after achieving stable control (pain relief and management of side effects) should one switch to extended-release formulations or other routes of administration, such as transdermal.
If an opioid analgesic proves ineffective, or if the patient shows significant intolerance (idiosyncrasy) or intolerable side effects, it should be switched to another, adhering to the principle of equianalgesia.
The starting doses for such opioid-naive patients should be minimal, followed by gradual increases. Suppose your patient was taking tramadol and is now transitioning to morphine. In that case, this patient is not considered opioid-naive, and the morphine dose can be calculated based on the tramadol dosage previously received. If the patient has no prior experience with opioids, you should start with the lowest dose and increase it as needed.
Opioid analgesic therapy should always start with 'pure' opioids rather than mixed formulations and always with short-acting drugs. Only after achieving stable control (pain relief and management of side effects) should one switch to extended-release formulations or other routes of administration, such as transdermal.
If an opioid analgesic proves ineffective, or if the patient shows significant intolerance (idiosyncrasy) or intolerable side effects, it should be switched to another, adhering to the principle of equianalgesia.
The Principle of Equianalgesia for Opioids
The principle of equianalgesia involves calculating the equivalent dose of an opioid analgesic that provides equal pain relief when switching between different analgesics. The analgesic potential should remain the same during the transition.
The principle of equianalgesia should be followed both within the same drug, using different routes of administration, and between different opioid and non-opioid analgesics.
When switching from intravenous short-acting morphine to oral administration, the dose should be tripled, and when switching from subcutaneous to oral administration, the dose should be doubled. Conversely, when switching from oral to subcutaneous, the dose should be halved, and from oral to intravenous, divided by three. For instance, if your patient receives 30 mg of morphine intravenously in an extended-release form and is discharged home where swallowing is restored and the tube is removed, you should triple the dose—30 mg becomes 90 mg of morphine, divided into six doses. If the patient received 30 mg subcutaneously, the required dose would be doubled to 60 mg of oral morphine, again divided into six doses per day. This principle applies to morphine as well as other drugs.
The principle of equianalgesia involves calculating the equivalent dose of an opioid analgesic that provides equal pain relief when switching between different analgesics. The analgesic potential should remain the same during the transition.
The principle of equianalgesia should be followed both within the same drug, using different routes of administration, and between different opioid and non-opioid analgesics.
When switching from intravenous short-acting morphine to oral administration, the dose should be tripled, and when switching from subcutaneous to oral administration, the dose should be doubled. Conversely, when switching from oral to subcutaneous, the dose should be halved, and from oral to intravenous, divided by three. For instance, if your patient receives 30 mg of morphine intravenously in an extended-release form and is discharged home where swallowing is restored and the tube is removed, you should triple the dose—30 mg becomes 90 mg of morphine, divided into six doses. If the patient received 30 mg subcutaneously, the required dose would be doubled to 60 mg of oral morphine, again divided into six doses per day. This principle applies to morphine as well as other drugs.
Main Opioid Analgesics
Tramadol
Tramadol is a μ-receptor agonist and a synthetic opioid analgesic with a central mechanism of action. It possesses antidepressant properties, suppressing the reuptake of norepinephrine by neurons and enhancing serotonin release, indirectly amplifying its analgesic effect. Tramadol is used for moderate pain (the second step of the WHO Pain Ladder).
Side effects (vary by individual, may or may not be pronounced): dizziness, nausea, vomiting, constipation (less severe than with morphine but still possible).
Tramadol affects serotonin metabolism and availability, potentially leading to serotonin toxicity, especially in elderly patients, and can lower the seizure threshold. As tramadol increases serotonin release, patients taking antidepressants may develop serotonin syndrome, so caution is necessary when combining tramadol with serotonin inhibitors.
Tramadol significantly reduces the analgesic effect in individuals with weak metabolism of cytochrome P450 2D6 (CYP2D6) and competes with this cytochrome, potentially increasing toxicity or reducing efficacy. Use cautiously with SSRIs and MAO inhibitors.
Tramadol has antitussive properties. Unlike morphine, it does not suppress respiration at therapeutic doses and has a lesser impact on gut motility. Its effects on the cardiovascular system are minimal.
Analgesic potential: 1/6 to 1/10 that of morphine. For instance, 50 mg of tramadol is approximately equivalent to 5 mg of morphine.
Available in capsules (50 mg), tablets (50 or 100 mg), and ampoules (100 mg).
Tramadol is a μ-receptor agonist and a synthetic opioid analgesic with a central mechanism of action. It possesses antidepressant properties, suppressing the reuptake of norepinephrine by neurons and enhancing serotonin release, indirectly amplifying its analgesic effect. Tramadol is used for moderate pain (the second step of the WHO Pain Ladder).
Side effects (vary by individual, may or may not be pronounced): dizziness, nausea, vomiting, constipation (less severe than with morphine but still possible).
Tramadol affects serotonin metabolism and availability, potentially leading to serotonin toxicity, especially in elderly patients, and can lower the seizure threshold. As tramadol increases serotonin release, patients taking antidepressants may develop serotonin syndrome, so caution is necessary when combining tramadol with serotonin inhibitors.
Tramadol significantly reduces the analgesic effect in individuals with weak metabolism of cytochrome P450 2D6 (CYP2D6) and competes with this cytochrome, potentially increasing toxicity or reducing efficacy. Use cautiously with SSRIs and MAO inhibitors.
Tramadol has antitussive properties. Unlike morphine, it does not suppress respiration at therapeutic doses and has a lesser impact on gut motility. Its effects on the cardiovascular system are minimal.
Analgesic potential: 1/6 to 1/10 that of morphine. For instance, 50 mg of tramadol is approximately equivalent to 5 mg of morphine.
Available in capsules (50 mg), tablets (50 or 100 mg), and ampoules (100 mg).
Tapentadol (Palexia)
I haven't worked with this drug, but it is known to be common in Russia and other countries. It is a synthetic analgesic, μ-receptor agonist, and norepinephrine reuptake inhibitor.
Tapentadol is used for nociceptive, inflammatory, neuropathic, and visceral pain. It undergoes significant metabolism, with approximately 97% glucuronidation. Tapentadol and its metabolites are almost entirely excreted by the kidneys (99%). The half-life is 5-6 hours, with a dosing regimen of 50 mg twice daily.
I haven't worked with this drug, but it is known to be common in Russia and other countries. It is a synthetic analgesic, μ-receptor agonist, and norepinephrine reuptake inhibitor.
Tapentadol is used for nociceptive, inflammatory, neuropathic, and visceral pain. It undergoes significant metabolism, with approximately 97% glucuronidation. Tapentadol and its metabolites are almost entirely excreted by the kidneys (99%). The half-life is 5-6 hours, with a dosing regimen of 50 mg twice daily.
Morphine
Morphine is quickly absorbed into the bloodstream regardless of the administration route, and the peak concentration depends on the route:
The duration of analgesia is determined by morphine's biotransformation in the liver, its elimination, and the genetically determined activity of its active metabolite.
Morphine suppresses the cough reflex and has notable antitussive properties. It stimulates chemoreceptors in the brainstem's trigger zones, causing nausea and vomiting.
Morphine does not cause clinically significant respiratory depression in cancer patients, as pain acts as a physiological antagonist to its central depressive effects. Thus, those with chronic pain do not typically experience respiratory suppression or develop dependency.
Significant side effect: respiratory centre depression related to reduced sensitivity to CO2. The peak depressive effect occurs at:
Gold standard for chronic cancer pain treatment: Morphine is a pure μ-receptor agonist, and its binding to peripheral and CNS receptors results in analgesia. The half-life for short-acting morphine is 4 hours; for extended-release forms, it's 8-12 hours. For patients with chronic kidney disease, the half-life may extend by 2.5 to 7.5 times.
For opioid-naive patients start with the minimum effective dose—2.5-5 mg orally every 4 hours for adults. For previously treated patients, initial doses of 10 mg short-acting every 4 hours can be used until a balance between analgesia and side effects is achieved. Have extra doses available for breakthrough pain. Once stabilised, switch to extended-release or alternative routes while observing equianalgesic principles.
Increasing dose for tolerance or other reasons: Increase the single dose by 30-50%. For instance, if the patient takes 10 mg every 4 hours, increase to 13-15 mg every 4 hours, equaling a total daily dose of 78-90 mg.
How to manage breakthrough pain with morphine? Assume you have achieved effective analgesia, and for the past 10 days, your patient has been on a stable dose of 90 mg of morphine per day with minimal or no pain. Suddenly, the patient reports that they are experiencing intense pain episodes that they can no longer manage. As we know, breakthrough pain can be spontaneous, more severe than baseline pain, and short-lived. It may be so intense that the patient finds it unbearable.
First, it is essential to correctly diagnose whether this is indeed breakthrough pain and determine whether it is related to the patient's underlying condition. If confirmed, the patient can be administered 50-100% of their single dose of short-acting opioids or 1/6 of their total daily dose of short-acting opioids. For instance, if the patient is on 10 mg of short-acting morphine, they may be given 5-10 mg to manage the breakthrough pain.
If the patient experiences more than 4-5 breakthrough pain episodes, the pain management strategy should be reviewed, and the total daily dose should be recalculated to include the additional opioid doses. For example, if the patient were taking 60 mg of short-acting morphine plus an additional 30 mg for breakthrough pain, the new total daily dose would be 90 mg. This should then be divided into six doses, resulting in a new single dose of 15 mg.
Tapering and discontinuing morphine: In cases where the patient's pain has subsided, such as following tumour reduction, discontinuing analgesia may be necessary. The morphine dose can be reduced gradually or discontinued by decreasing the total daily dose by 25-30% every 2-3 days to avoid withdrawal symptoms (abstinence syndrome).
Morphine is quickly absorbed into the bloodstream regardless of the administration route, and the peak concentration depends on the route:
- 7-10 minutes for intravenous;
- 30 minutes for subcutaneous;
- 60 minutes for oral.
The duration of analgesia is determined by morphine's biotransformation in the liver, its elimination, and the genetically determined activity of its active metabolite.
Morphine suppresses the cough reflex and has notable antitussive properties. It stimulates chemoreceptors in the brainstem's trigger zones, causing nausea and vomiting.
Morphine does not cause clinically significant respiratory depression in cancer patients, as pain acts as a physiological antagonist to its central depressive effects. Thus, those with chronic pain do not typically experience respiratory suppression or develop dependency.
Significant side effect: respiratory centre depression related to reduced sensitivity to CO2. The peak depressive effect occurs at:
- 7-10 minutes post-intravenous administration,
- 30 minutes post-intramuscular administration,
- 60-90 minutes post-subcutaneous administration of a therapeutic dose.
Gold standard for chronic cancer pain treatment: Morphine is a pure μ-receptor agonist, and its binding to peripheral and CNS receptors results in analgesia. The half-life for short-acting morphine is 4 hours; for extended-release forms, it's 8-12 hours. For patients with chronic kidney disease, the half-life may extend by 2.5 to 7.5 times.
For opioid-naive patients start with the minimum effective dose—2.5-5 mg orally every 4 hours for adults. For previously treated patients, initial doses of 10 mg short-acting every 4 hours can be used until a balance between analgesia and side effects is achieved. Have extra doses available for breakthrough pain. Once stabilised, switch to extended-release or alternative routes while observing equianalgesic principles.
Increasing dose for tolerance or other reasons: Increase the single dose by 30-50%. For instance, if the patient takes 10 mg every 4 hours, increase to 13-15 mg every 4 hours, equaling a total daily dose of 78-90 mg.
How to manage breakthrough pain with morphine? Assume you have achieved effective analgesia, and for the past 10 days, your patient has been on a stable dose of 90 mg of morphine per day with minimal or no pain. Suddenly, the patient reports that they are experiencing intense pain episodes that they can no longer manage. As we know, breakthrough pain can be spontaneous, more severe than baseline pain, and short-lived. It may be so intense that the patient finds it unbearable.
First, it is essential to correctly diagnose whether this is indeed breakthrough pain and determine whether it is related to the patient's underlying condition. If confirmed, the patient can be administered 50-100% of their single dose of short-acting opioids or 1/6 of their total daily dose of short-acting opioids. For instance, if the patient is on 10 mg of short-acting morphine, they may be given 5-10 mg to manage the breakthrough pain.
If the patient experiences more than 4-5 breakthrough pain episodes, the pain management strategy should be reviewed, and the total daily dose should be recalculated to include the additional opioid doses. For example, if the patient were taking 60 mg of short-acting morphine plus an additional 30 mg for breakthrough pain, the new total daily dose would be 90 mg. This should then be divided into six doses, resulting in a new single dose of 15 mg.
Tapering and discontinuing morphine: In cases where the patient's pain has subsided, such as following tumour reduction, discontinuing analgesia may be necessary. The morphine dose can be reduced gradually or discontinued by decreasing the total daily dose by 25-30% every 2-3 days to avoid withdrawal symptoms (abstinence syndrome).
Opioid Rotation
Replacing one opioid with another may be warranted and necessary in the following cases:
- Genetically determined individual intolerance related to specific opioid receptor characteristics;
- The occurrence of intolerable side effects that prevent dose escalation to achieve adequate pain relief;
- Ineffectiveness of an opioid, such as when tramadol reaches its toxic dosage limit and 400 mg of tramadol becomes ineffective, necessitating a switch to a different medication;
- Patient preferences, issues with swallowing, and other technical reasons. For instance, if a patient finds it difficult to take medication every 4 hours or to adhere to a strict schedule, transitioning to an extended-release form of the drug can be considered once stable pain control is achieved.
Webinar PACED
The graph shows the peak concentration for intravenous administration, represented by the red line, occurring within 7-10 minutes. There is almost no plateau phase here: it rises sharply and gradually falls. The blue line represents subcutaneous administration, showing a slight plateau after 30 minutes. Finally, the yellow line represents oral administration, where the drug remains in the plateau phase longer, with the plateau occurring 60 minutes after intake.
Webinar PACED
If we administer 20 mg of morphine to a patient, after 4 hours, only 10 mg, or 50% of the drug, remains in the body. At this point, the next dose should already be administered rather than waiting for 100% elimination of the drug. This is crucial because, without a period of analgesia absence (Figure 1: below the 10 mg line), the plateau extends — which is what we aim for.
Figure 2 shows the first, second, third, and so on administrations. Only after 4-5 half-life periods can we reach the peak concentration and assess whether our dose is effective. This process takes between 16 and 20 hours, thus stabilising the drug concentration in the body.
Figure 2 shows the first, second, third, and so on administrations. Only after 4-5 half-life periods can we reach the peak concentration and assess whether our dose is effective. This process takes between 16 and 20 hours, thus stabilising the drug concentration in the body.
Opioid Antagonist Naloxone
If you are using opioids, it's essential to always have naloxone on hand. Naloxone is an opioid antagonist used to block or reverse the effects of opioid drugs, especially in cases of overdose.
Naloxone has a high affinity for μ-opioid receptors, acting as an inverse agonist, rapidly displacing any other drugs bound to these receptors.
Naloxone is used to restore breathing after an opioid overdose involving drugs like morphine, hydromorphone, methadone, heroin, or fentanyl. The effect appears within 2 minutes for intravenous administration, 5 minutes for intramuscular injection, and 10 minutes after nasal spray administration. Important Note! If a patient is using a fentanyl patch and experiences respiratory depression, remember that the action of naloxone is temporary! Naloxone blocks the effect of opioids for only 30-90 minutes.
In Armenia, naloxone is registered and effectively used. However, if this is not the case in your country, there is an alternative method. Since the kidneys excrete morphine, if an overdose is suspected, diuretics can be prescribed to the patient, helping eliminate the excess through urine.
Naloxone has a high affinity for μ-opioid receptors, acting as an inverse agonist, rapidly displacing any other drugs bound to these receptors.
Naloxone is used to restore breathing after an opioid overdose involving drugs like morphine, hydromorphone, methadone, heroin, or fentanyl. The effect appears within 2 minutes for intravenous administration, 5 minutes for intramuscular injection, and 10 minutes after nasal spray administration. Important Note! If a patient is using a fentanyl patch and experiences respiratory depression, remember that the action of naloxone is temporary! Naloxone blocks the effect of opioids for only 30-90 minutes.
In Armenia, naloxone is registered and effectively used. However, if this is not the case in your country, there is an alternative method. Since the kidneys excrete morphine, if an overdose is suspected, diuretics can be prescribed to the patient, helping eliminate the excess through urine.
Webinar PACED
This table shows the ratio of different opioid drugs. There is a rule: if you are recalculating from one opioid analgesic to another, the new one should be reduced by 50% until one reaches the required concentration.
Q&A Session
Question 1
In your opinion, what is the main obstacle to opioid pain management:
- ophidiophobia, which is often present among both specialists and patients;
- lack of knowledge among doctors who are afraid to use complex drugs;
- fear of consequences in case of errors — primarily legal issues, such as prosecution due to incorrect record-keeping or loss of a capsule;
- infrastructural challenges: not all pharmacies sell opioids, or these drugs may not be available in the country at all?
Narine Movsesyan
The question itself answers it. Everything you listed is a significant barrier to opioid pain management. But primarily, it’s the mentality — that’s the most challenging part. Changing deeply ingrained beliefs is hard. I'm sure our population, and not just ours, often gets information from movies, TV shows, and other secondary sources far from reality. I always emphasise that opioids are pain-relief medications. We need to talk about this and read up on it. I work with PACED, an organisation that helps us promote the use of opioids. We conduct training seminars and have already completed three rounds across all regions of Armenia. We reach people so that no one can say, 'I'm the only doctor here; where would I go to learn?' We bring knowledge to them and then conduct follow-ups.
Doctors should ideally know the most about prescribing opioid analgesics. Still, sometimes they avoid this problematic drug and discourage patients by saying they don’t need it, or it’s only used at the last stage when the patient isn’t at that stage, and so on. We address all of this through education and courses. Our state postgraduate program includes a pain management course. We also use social platforms, street events, and appearances to combat the stigma attached to the word 'narcotic.' These are complex drugs that require expertise, but I believe if you don’t continue educating yourself, you shouldn’t be prescribing at all.
Question 2
How do you conduct conversations with patients or their relatives about transitioning to opioid analgesics? At what point does this conversation happen: when moving from the first to the second step or from the second to the third, involving more potent opioids?
Narine Movsesyan
These conversations are tough. A patient might not even know they have a malignancy; they come for treatment and hear that their illness is incurable and they need morphine. I try to establish close contact with the patient, gradually explaining step by step that there is a disease, a symptom that requires specific treatment, that the medications they were using before won’t work and will continue to cause suffering, so opioids are necessary. Many start asking if they can stay on nonsteroidal anti-inflammatories. I explain that complications could develop, bringing new and more severe issues than painkillers at the doses I prescribe with all precautions, etc.
I also emphasise that it doesn’t matter what stage the disease is at. People often associate opioids with the final days of life. Some doctors mistakenly think so, too. Morphine is a pain-relief medication. Patients are usually reassured when I say, 'You came for chemotherapy. During this treatment, the tumour will shrink, the pain will decrease, and we will take you off strong painkillers. This is not a death sentence.' And they relax. I tell them we can always reduce the dose. Then, the patient adapts and realises that it helps them. You shouldn’t go against a patient’s will; you must ensure they work with you, not break them, but collaborate.
Providing information and thorough explanations — however much the patient needs to understand everything. It’s essential to communicate in a language they understand, whether a child, an older person, or someone who doesn’t know where they are and what they’re doing. Communicate in an accessible language.
Question 3
Have there been cases in your practice where patients or their families, despite multiple explanations, categorically refused the use of opioid analgesic drugs until the end, until the patient's death? Does the fact that you cannot use these drugs without consent demoralise you? How do you handle this?
Narine Movsesyan
Why do palliative care doctors often experience burnout? Because they constantly have to go against the current. Everything is against you, and you have to live with it somehow.
I have rarely encountered such cases. In individual cases, I hold additional conversations with the family members. I don’t try to force them or go against them; I interact with them. I explain that I have a way to help, and if there were another option, I would use it, but there isn’t. Communication needs to be so well-established that it overcomes these prejudices. Sometimes, if it comes down to the family, I may tell them they are taking responsibility for the patient's suffering. If the resistance continues, I absolve myself of any responsibility. What else can we do? But that is after I’ve exhausted all my options.
The patient or their representative must take responsibility to help them understand the gravity of their decisions. This is the last argument, yes. It may be somewhat manipulative, but what can you do if there are no other options and the person is suffering because of someone's biases?
Question 4
How do you assess pain in a patient who, due to their condition, cannot express their pain? What tools or scales do you use?
Narine Movsesyan
I have had several such cases. It’s important to remember that verbal expression is just one way to indicate pain. There are also behavioural signs, such as facial grimacing and unusual patient behaviour. Often, family members notice changes, such as explosive movements or unexplained crying.
I had an interesting case with a breast cancer patient who needed morphine, but the clinic doctor wouldn’t prescribe it because she didn’t believe the patient was in pain. The patient, who was in her fifties, had early Alzheimer's. She had a calm, even serene expression. She couldn’t report her pain herself, so I asked the family why they believed she was in pain. Her daughter-in-law said that when touched or bathed, the patient would push away, fight, and howl. While we talked, the patient sat quietly next to us. I examined her—her ribs were infiltrated and very painful. The moment I touched her, she flinched and tried to pull away. Behavioural reactions help us gauge pain when speech isn’t available. Especially when caretakers report changes in behaviour, it’s a signal to consider if the patient is in pain.
There is no specific scale for such cases, but for early-stage Alzheimer's or minor cognitive impairment, I ask simple questions: Does it hurt, yes or no? Where does it hurt? Does it hurt here? Or there? It’s about identifying potential pain points based on the patient's condition.
The most reliable way to check is simply to administer pain relief. Suppose you give an analgesic at the peak of unusual behaviour, whether it's metamizole or another non-opioid, and the patient calms down. In that case, it strongly indicates that pain was the cause.
You shouldn’t use opioids for such tests unless there are direct complaints of pain. The goal is to determine if the issue is pain or something else, like delirium or a psychotic episode. It could be as simple as thirst or discomfort. Rule out other possibilities and try a non-opioid analgesic to see if the person calms down within a reasonable time. If they do, it’s likely a pain; if not, investigate further.
As we assess pain in children using scales and observing behaviour, the same applies to elderly or Alzheimer's patients. You might see unusual behaviour, increased blood pressure, or tachycardia — test with a non-opioid analgesic to check for pain.
Question 5
Some say that the U.S. is experiencing a crisis of 'over-pain management' with systems like morphine pumps that allow patients to self-administer doses. There is no set schedule or monitoring by specialists; patients regulate their pain management themselves. What’s your opinion on this method, and would it be worth implementing in Armenia?
Narine Movsesyan
Patient-controlled anaesthesia is convenient for the postoperative period. When a patient feels pain, they press a button to get a dose of morphine. Of course, there are built-in safety measures to prevent overdosing.
In Armenia, our patients use oral morphine and have constant access to it. There are systems like 'butterfly' needles and specialised syringes, but we don’t have those in Armenia. I wish we did; it would be more practical for patients who struggle to swallow or follow a medication schedule. With such a system, the patient would have a subcutaneous needle and just need to press a button. It’s a purely technical issue, but I think it’s a convenient option, especially for patients discharged home at a stage where pain relief is their primary need.

